For patients on dialysis, time is valuable — whether at work, or with friends and family, every moment counts. While in-clinic dialysis has long been the default for care, it means that patients spend time and money, travelling to and from a fixed schedule of appointments.
But there’s a change afoot.
Home dialysis is offering patients across the region with a different option. To make it happen, a team of experts at Kingston Health Sciences Centre (KHSC) is working hard to provide vital equipment and training so patients can safely and independently perform their own treatments at home, for free.
“It’s such a huge improvement in quality of life,” says Lori Van Manen, Director of the Regional Renal Program. “Home dialysis has less impact on their life because patients don’t have to come to the hospital three times a week for treatments that each take four hours to complete.”
Removing barriers
There are two options for home dialysis: Home hemodialysis (HHD) and Peritoneal dialysis (PD). Patients or their caregivers typically manage treatments at home independently, but for those who need a little extra help, there’s the Home Dialysis Assistance Program (HDAP).
HDAP is a collaboration between the hospital and local service providers that adds an extra level of support by coordinating home visits by a nurse or PSW. These care providers visit patients at home once-or-twice a day to help with any parts of treatment they may otherwise struggle with, like setting up their dialysis, or cleaning up after their treatment is finished. Care can be short-term or ongoing, depending on the patients’ needs.
It’s a unique service in southeastern Ontario and part of the bigger KHSC @ Home program – a regional partnership that helps patients transition out of hospital and back into their homes.
“In-centre dialysis doesn’t need to be the default treatment due to logistical barriers with home dialysis,” says Anne Dumais, Program Manager. “HDAP is an extra, optional level of care that helps clear those barriers and open up new possibilities.”
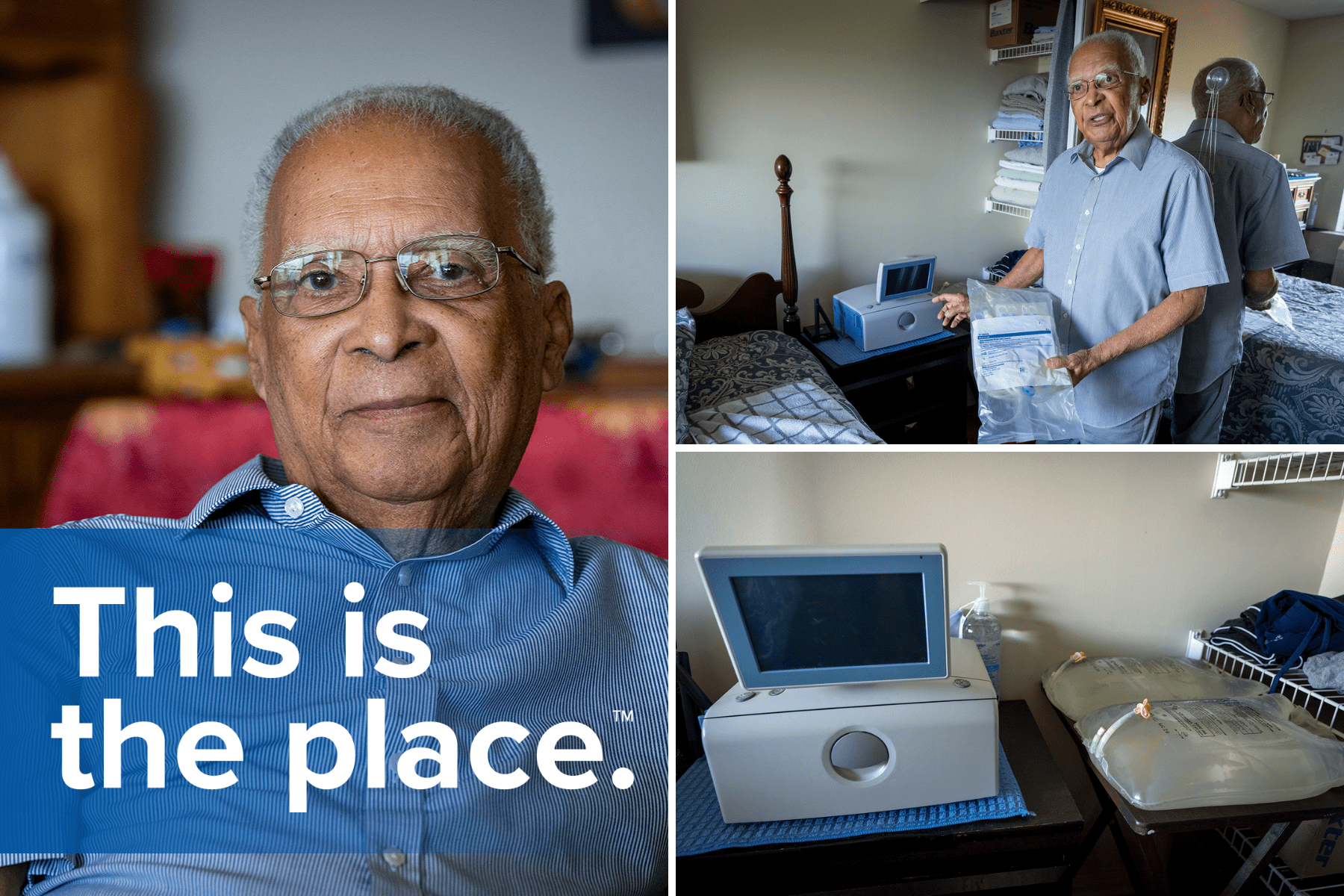
Currently, 37 home PD patients are receiving help through HDAP. Dr. Philippe Craan is one of them. He’s been a dialysis patient at KHSC for four years and, as a retired physician, has a unique perspective.
“I can speak as both a patient and a physician when I say my experience has been excellent,” says Dr. Craan, who graduated from medical school in Geneva, 55 years ago, before moving to Ontario to practice. “They work with you to design an individual program that helps to get the toxins out of your bloodstream.”
Don't’ worry - you don’t need to be a physician to make home dialysis work. Dr. Craan acknowledges that the formula is simple: it just takes time, education, and patience to get the process right.
He was able to independently manage his home care for three years, until an injury last year meant he could no longer move the 25lb bags of dialysis fluid involved in treatment. It could’ve meant that in-centre dialysis was his only option, but HDAP was there to help. Now a nurse visits every morning to help.
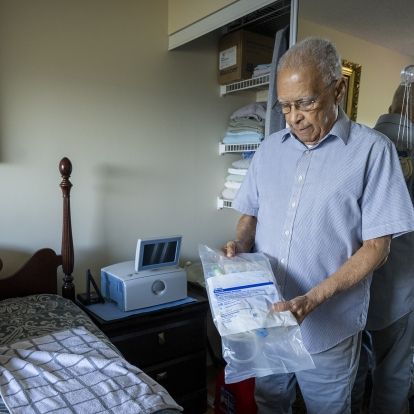

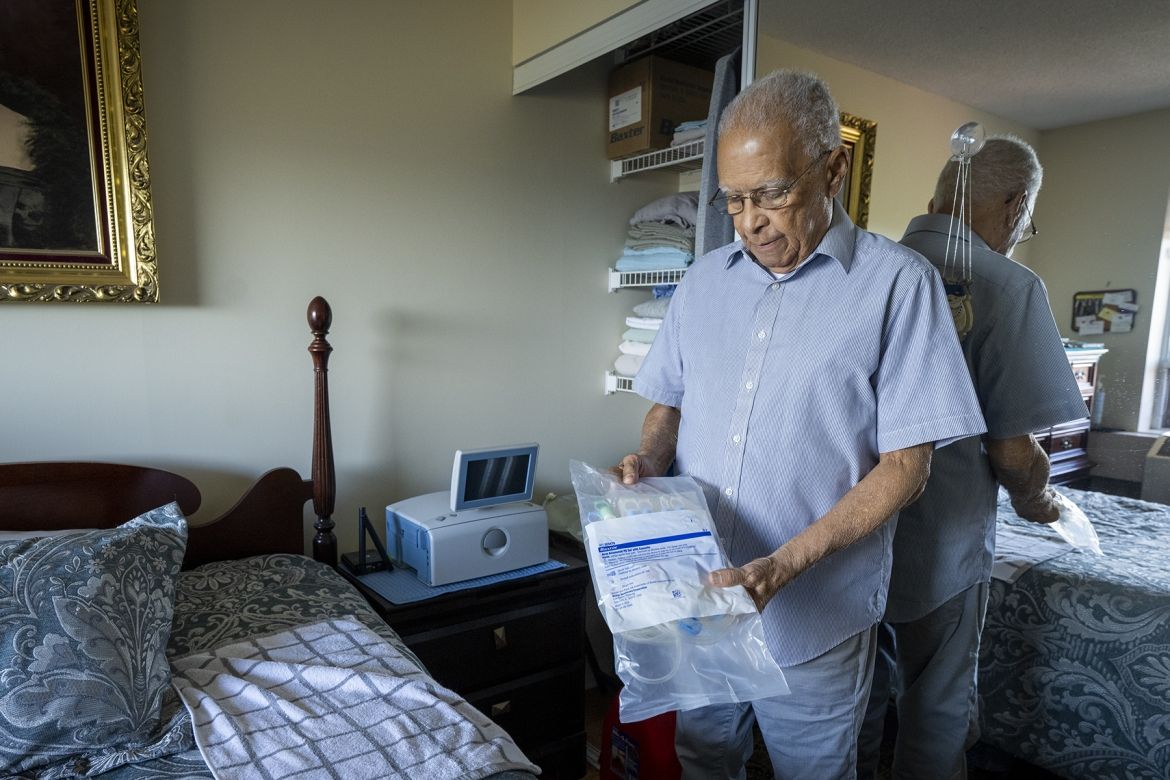
Dr. Craan showing some of the different components that make up his routine dialysis treatment.
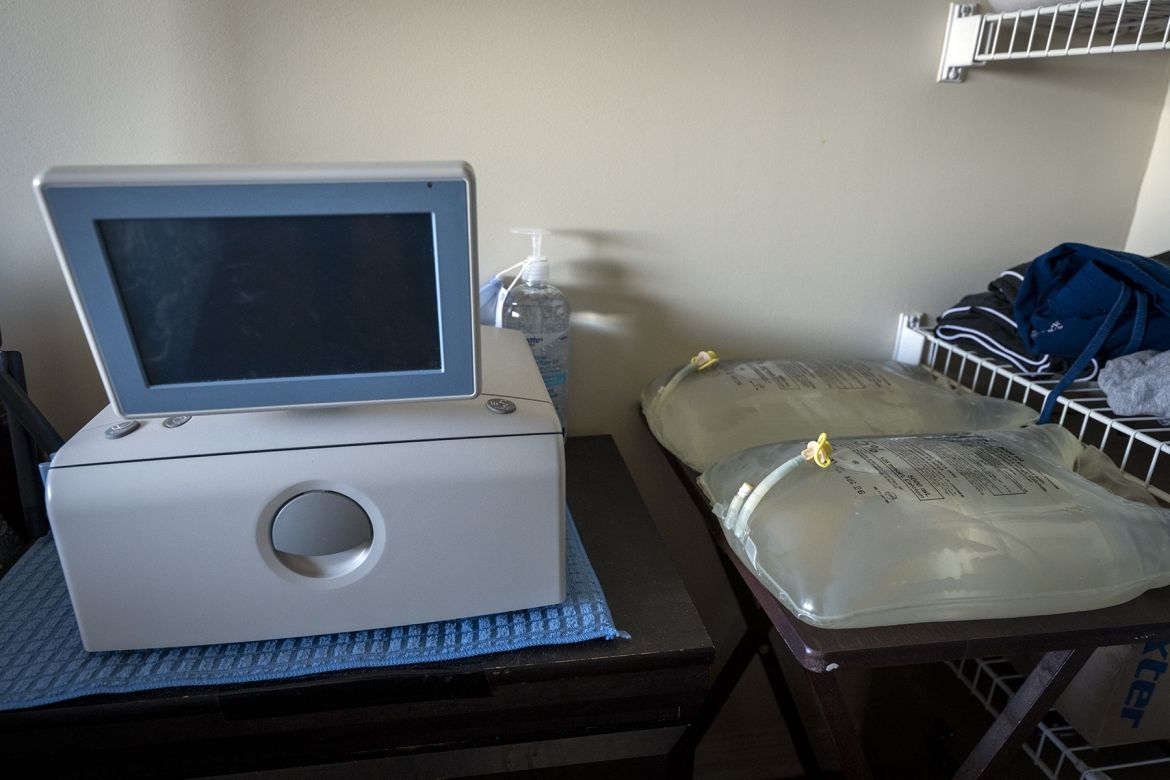
The advanced dialysis "cycling" machine next to the dialysis fluid used for treatments.
“I have no problem with connecting myself, maintaining the catheter and other parts of treatment – I'm used to that. But the extra help is valuable to get everything ready.”
Meeting patients, and families, where they are
When Denise Carquez’s husband, Rick, contracted COVID-19 in early 2024, his kidney function declined rapidly.
“It caused a panic,” says Denise, reflecting on the experience. “Suddenly, his [kidney] numbers were way off, and we had to move fast to get him set up on dialysis. The [Renal] program rallied to get things set up quickly and they’ve been great with support ever since.”
Rick started treatment in March. Home dialysis was the best fit because it tends to be easier on the heart, which extra is important since Rick had a heart transplant in 2017. It also means he can be involved in daily routines like taking their nine-year-old son to school every morning.
Considering the alternatives, Denise agrees. “The stress of heading downtown for daily in-centre treatment wouldn’t have worked for him. It just wouldn’t.”
Because her husband often has brain fog – a common side-effect of dialysis - Denise helps with treatment. She connects him every night, but cleaning and preparing the equipment can be a full-time job on its own. Without HDAP, either Rick would need to do in-centre dialysis or Denise would no longer be able to work.
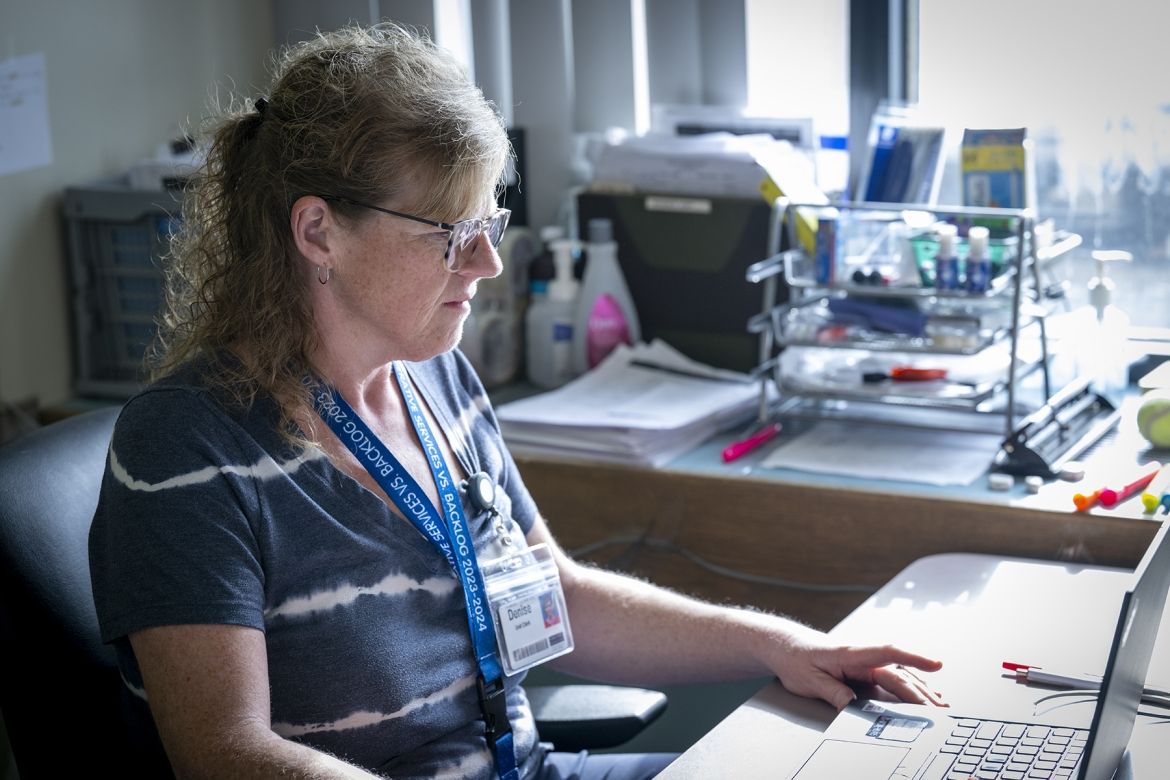
Thanks to HDAP, it’s one less thing to worry about. She can continue to work as a clerk with KHSC’s Virtual Recovery after Surgery Program – something that’s important to her personally – while nursing staff assist with setup and cleaning at home.
“[Rick] sometimes feels like a burden, but he’s not. I signed up for this. I agreed to do this. He gets to spend more time with his family, and you don’t get that leeway with in-centre dialysis.”
For Denise and her family, that means more time spent together. This year the Carquez family was able to go on five camping trips and, because peritoneal dialysis supplies can be shipped to different vacation locations, they’re now planning a family trip abroad.
By adjusting routines and expectations, HDAP can help make sure patients are getting the dialysis care they need at home in a way meets their needs.