Effective immediately masking is required for everyone when present on all inpatient units, in the Emergency Department (ED), the Urgent Care Centre (UCC), and the Children’s Outpatient Centre (COPC).
KHSC In-depth: Unmasked
Hannah Green, Critical Care Nurse
Hannah Green has worked at Kingston Health Sciences Centre for 11 years. She’s been in the ICU for more than five. She’s also pregnant, now in her third trimester.
While she isn’t currently caring for COVID patients as a precaution during her pregnancy, she continues to come to work in the ICU to provide care to some of the sickest patients in the region.
“Some of my friends and family want me to take time off work, but I don’t want to stop working just because of COVID,” she says. “We’re so short staffed across the province, I feel bad because I want to help my colleagues. You feel guilty on one hand and scared on the other, but it does make me feel a little bit better that we still have non-COVID patients in the ICU that I can work with.”
She was drawn to critical care nursing because of the complexity of the patients in the ICU, the intensity and teamwork required to care for them. But that intensity has only increased during the third wave.
“Normally you’re tired because you’re on your feet for long shifts, it’s physical. But now it’s more emotional. Seeing death is part of working in an ICU and we have a lot of cases where it’s predicted but it takes time. With many of these COVID cases it’s quick, just a couple of days. We did everything we could but there was no way to stop it, no way to prevent it. Sometimes it’s so quick that the family doesn’t have enough time to fully grasp what’s happening before their loved one has passed away.”
She says many of the patients they’re seeing are a lot younger than the ‘typical’ ICU patient, some of them in their 20s and 30s. They’re from diverse cultural backgrounds, they’re essential workers living in multigenerational homes. They’ve done nothing ‘wrong’ to catch COVID-19.
“They are going to be in the hospital for a long period of time, I expect many will be here for months. The ICU is filling up because people are still having heart attacks and car accidents and we need to care for them too. That’s what is stressful, this is the way it’s going to be for a long time.”
“I really don’t think public fully understands. I go on social media and see some of the comments and it’s disheartening to see the anti-mask and anti-lockdown rallies. It’s hard because you know that a lot of people won’t grasp what’s going on until someone they know is in the hospital.”
Sarah Stanley, Respiratory Therapist
If you ever need help breathing, chances are you’ll be under the care of a Respiratory Therapist (RT) like Sarah Stanley. The mother of three has been busy balancing her kids’ virtual learning during the day and 12-hour overnight shifts in the ICU.
“I try to fit in a nap in the afternoon if the kids let me,” she says. “I recently had three days off in a row and didn’t even feel halfway rested. It’s tiring.”
She estimates that at KHSC there are more than 50 RTs who support patients across the hospital. Their patients run the gamut from those who need simple nasal oxygen all the way to those who need a ventilator to breathe. With the influx of COVID patients at KHSC, the number of vented patients that require the help of her team has doubled.
“I can’t give our small department enough praise at the moment. We started planning for this last year, we did practice simulations to make sure we were really well prepared. While we didn’t see much through the first and second wave, I knew we couldn’t get through the third wave being so lucky. It’s been inspiring to be at work to see how everyone in the critical care team has come together to deliver this care.”
In the ICU, she says their COVID patients are mostly sedated so their bodies don’t reflexively fight against the ventilators. The team then has to ensure that enough oxygen gets into the blood and enough carbon dioxide is removed.
“It’s a fine line where we breathe for them, but not hurt their lungs by doing too much because they have been damaged by the virus. You have to think on your feet, we constantly weigh the balance of having to do more with the ventilator as they get sicker but not risk causing damage.”
“These are the patients that we are trained to care for, but they’re so sick. The scale and the duration of this is emotionally exhausting. We are going from patient to patient, trying to do our best, but at the end of the day it hits you pretty hard.”
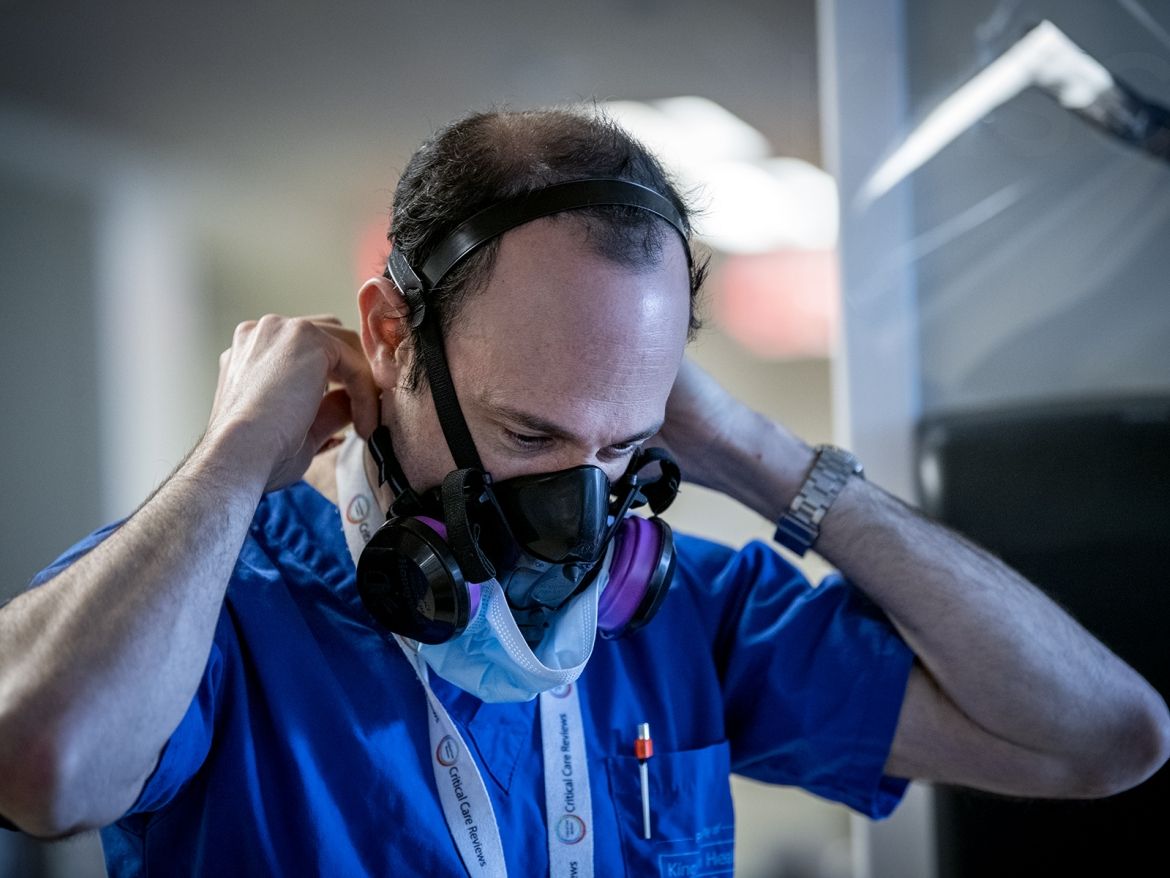
Dr. David Maslove, Critical Care Physician
Even at the best of times, Kingston’s ICUs are busy. But they’ve gotten busier. Over the last few months the number KHSC’s critical care beds has increased from 65 to more than 100, in an effort to create capacity in Ontario to care for the growing number of COVID-19 patients.
Dr. David Maslove, who trained in critical care medicine at Stanford University before relocating to Kingston, calls the current pace ‘taxing.’
“It’s definitely busy, much busier than usual. We now need to get more done in the same amount of hours.”
Having been largely spared by the first and second waves in Ontario, KHSC was able to take time to undergo pandemic planning across multiple departments, which has allowed the organization to support other regions of the province.
“It’s been heartening to see how incredibly well our team has come together to provide support for these patients. I knew this was a great group to work with, but to see it come together like this has been wonderful. It’s made the work go as smoothly as possible. I give immense credit to all the staff at the bedside 24/7; it’s been remarkable to watch.”
However, he acknowledges that despite how well the entire team is functioning, their COVID patients can be incredibly difficult to care for.
“They are very sick, amongst the sickest we have in the ICU at any one time. It’s been very eye opening to see, their lungs are so severely impacted that it’s challenging to treat.”
And with their families hundreds of kilometres away, communication to those loved ones back home creates an added layer of emotional output.
“We’ve long recognized caring for critically ill patients means caring for their families as well, so normally we have open policies for visitation. But these changes have been difficult, it’s hard for the people at the bedside to put themselves in the shoes of the families and it’s hard for the families to put that level of trust into people they’ve never met.”
“I’ve found it helpful to make those phone calls back to families in the afternoon where it gives you a moment to catch your breath and prepare for some difficult conversations. The emotions hit you a little harder at the end of the day when you have a chance to get some perspective on how big the challenges are for the families. It’s amazing and heartwarming to see the leap of faith these families are making.”
John Hoag, Patient Care Assistant
John Hoag credits his work ethic to having grown up on a farm. That dedication to getting the job done has served him well for the last 15 years working in the ICU.
“ICU isn’t the place to relax, even during more normal times,” he says. “Over the last two weeks I think I have worked over 100 hours, just to try and help with this surge. I had to take a couple of days off recently because I needed to slow down or I was going to crash.”
That pace, along with a balancing act at home, being a Dad to two sons, has required him to find balance.
“I’m happy to work those long hours as long as I don’t miss time with my kids. Their mom also works in the hospital as a nurse, so on my days off I have the boys and I need to be able to go home and be a dad. Although I will admit, I’m not doing a ton of work projects at home right now. Just trying to rest and recuperate, but having teenagers, they’re cool to just hang out and watch a movie.”
As a Patient Care Assistant, he acts like a Swiss army knife of sorts in the ICU. He assists with turning patients multiple times a day to improve their breathing, running for supplies, bathing patients, providing CPR, and just generally doing everything he can to make sure the unit runs as smoothly as possible.
“We’ve had some challenges in the ICU, but we’re always working to find creative solutions to those problems. For example if you’re working with a patient and you run out of a supply, you can’t just walk out and get more because of all the infection control precautions. So you need to always make sure you are prepared. Everything takes longer than usual and it’s mentally exhausting. You don’t want to make a mistake. But we’ve gotten very good at this in a hurry.”
“I am worried though about what this is doing to some members of our team emotionally who haven’t had as much time to develop coping mechanisms as the more veteran staff have. But, I’ve been teary eyed myself many times, never in front of my coworkers though. It’s been difficult, but I love this place and never plan on leaving.”
Fran Berrigan, Volunteer
Volunteering is in Fran Berrigan’s DNA.
“I think there is a volunteer gene and I got it from my mother. I worked my whole life, so the idea of having nothing productive to do after I retired was scary. I wanted to volunteer and when I moved to Kingston from Quebec I was drawn to the hospital, specifically the ICU.
While many volunteer programs were suspended across the hospital due to the pandemic, volunteers were allowed to continue coming to the Kidd 2 ICU.
“I just kept coming. It was a personal decision and I felt that I could be of help and support. Management was very supportive of that so here we are a year later.”
Berrigan is dedicated to her volunteer role, working four-hour shifts six days a week. Before the pandemic she focused on providing support to families in the waiting area outside of the ICU.
“The volume of visitors is down because of restrictions in place, but the role is still the same. Very often family members just need to sit and talk. I am here every morning so I can get to know them and we can talk about their dogs or something else in their lives to take their minds off it.”
Over the last year though, she has found that her role has shifted to also focus on providing comfort to the critical care staff as well.
“We have a nice large waiting area, so staff can use it for breaks now that there aren’t as many visitors. So I spend time with them, being a little sense of normal. I don’t know anything about ventilators, so we can talk about different things, just to give them a little break and talk about normal life to help ease their stress.”
“It has been a privilege for me to work with these people, this is my work family and knowing what they are going through this past year has been hard. I know they don’t have a choice to be here, and I do, so I choose to come in and help. I think some of the community doesn’t have a full appreciation of what the staff is going through. I was impressed with them before and am even more so now. They are doing an amazing job.”