Effective immediately masking is required for everyone when present on all inpatient units, in the Emergency Department (ED), the Urgent Care Centre (UCC), and the Children’s Outpatient Centre (COPC).

As the volume of people presenting with a mental health crisis steadily ramps up in the Emergency Department (ED) at Kingston Health Sciences Centre (KHSC), a new pilot project aimed at managing capacity and improving flow for these patients is quickly yielding positive results.
“Over the past six years we’ve seen a 50 per cent jump in patients arriving with mental health issues in the ED compared with 25 per cent rise in overall ED volumes,” says Carol McIntosh, Program Operational Director for Emergency and Ambulatory Services.
“On any one day, mental health-related visits account for 20 per cent of patient volumes, and half of those patients need a Psychiatry consult. Given our limited physical space and associated staffing levels, keeping pace with these volumes is a real challenge.”
Enter the Mental Health Nurse Navigator project.
Launched in mid-December to help largely with the expected Christmas surge in mental health visits, the joint ED-Mental Health Program project deploys an experienced Mental Health Nurse Navigator to the ED weekdays from 3 to 11 p.m., when mental health visits typically surge.
In the pilot model, patients move directly from Triage to the Nurse Navigator, who then coordinates their mental health care with ED physicians, psychiatrists, Social Work and the on-site crisis service.
As a result, patients are spared a long wait for an ED physician and their care plans, which can range from medication adjustment to outpatient or community referrals to admission, are initiated that much faster. In some instances, intervention by the ED physician may not even be required.
“This model of care is about getting these patients the help they need as quickly as possible,” says Michelle Matthews, Program Operational Director for Mental Health.
“The success of the Nurse Navigator hinges on a team effort in the ED, which includes strong support from highly skilled Social Workers. Everyone is focused on keeping things moving for the patient, which can reduce wait time and provide better access to community supports that decrease the chance of hospital admission.”
The project’s preliminary results have been positive. Introducing the role of a Mental Health Nurse Navigator has cut the time to initial assessment by the ED physician by 50 per cent and the average ED length of stay by 40 per cent for patients presenting with mental health issues.
While our Phase 2 redevelopment plan includes more ED space for mental health patients, the Emergency and Mental Health Programs are continuously exploring ways of streamlining their stay in the ED.
“We’re facing capacity issues with this patient population now,” says McIntosh, “so we keep looking at options that will let us provide the best care while optimizing our space and resources.”
Gallery

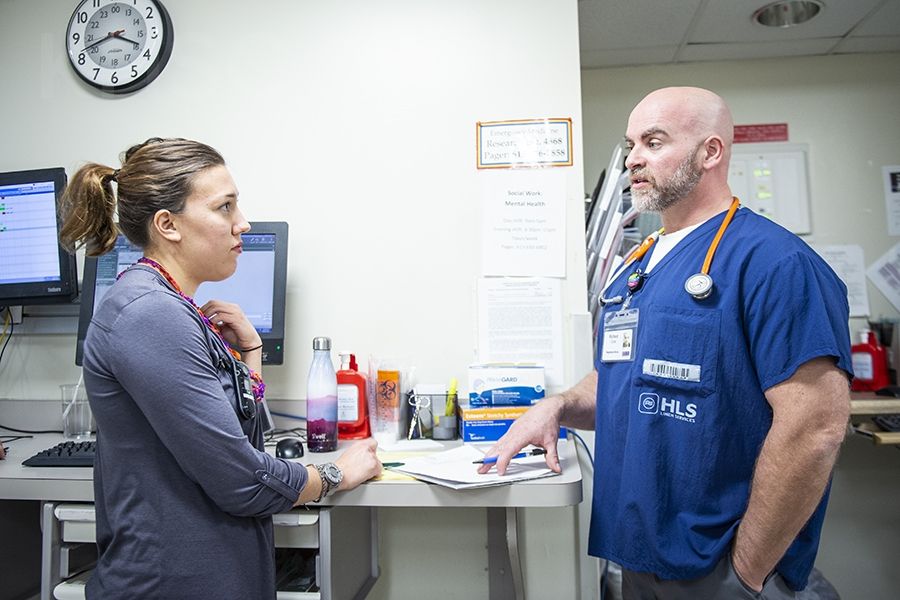
In his pilot role as Mental Health Nurse Navigator in the ED, Richard Cook, right, works closely with Social Worker Sarina Cormier, left, and other members of the ED team to speed up treatment and reduce wait times for patients with mental health emergenc