When kids are struggling with their mental health, hospital care can be a lifeline. But for some young patients, especially those who are neurodivergent, that care needs to look a little different.
That’s why Kingston Health Sciences Centre (KHSC) has added something new to its mental health team: two registered behaviour analysts who are already making a big difference in how care is delivered to kids who think and learn differently.
“It’s all about helping patients succeed, not just while they’re receiving inpatient or outpatient care, but when they are in their home communities,” says Melanie Darling, program manager for KHSC’s Child and Youth Mental Health program.
A community idea sparks lasting change
This powerful change started in 2023 with a simple conversation.
“A community member came to us with a desire to do something that would truly make a difference for kids with complex mental health needs,” Darling explains. "Together, we explored what was possible, and one of the things we landed on was adding a new team member to enhance the services available within the program."
Thanks to this generous donor through the University Hospitals Kingston Foundation, the behaviour analyst role was funded for a one-year pilot. The impact of the position was evident, leading to KHSC securing permanent funding.
What is neurodiversity?
Neurodiversity is a way of understanding the natural variations in how people think, feel, and experience the world. It includes conditions like autism spectrum disorder, attention deficit hyperactivity disorder, and fetal alcohol spectrum disorder.
Many patients come into KHSC’s Child and Youth Mental Health program needing specialized support, and now, that support is even stronger.
The difference a behaviour analyst makes
KHSC already had behaviour science technologists on the team, specialists who work one-on-one with kids to help them build coping skills and manage their emotional responses in certain situations. Registered behaviour analysts complement that care with in-depth assessment, long-term planning, skills development, and goal setting that continues beyond the hospital stay.

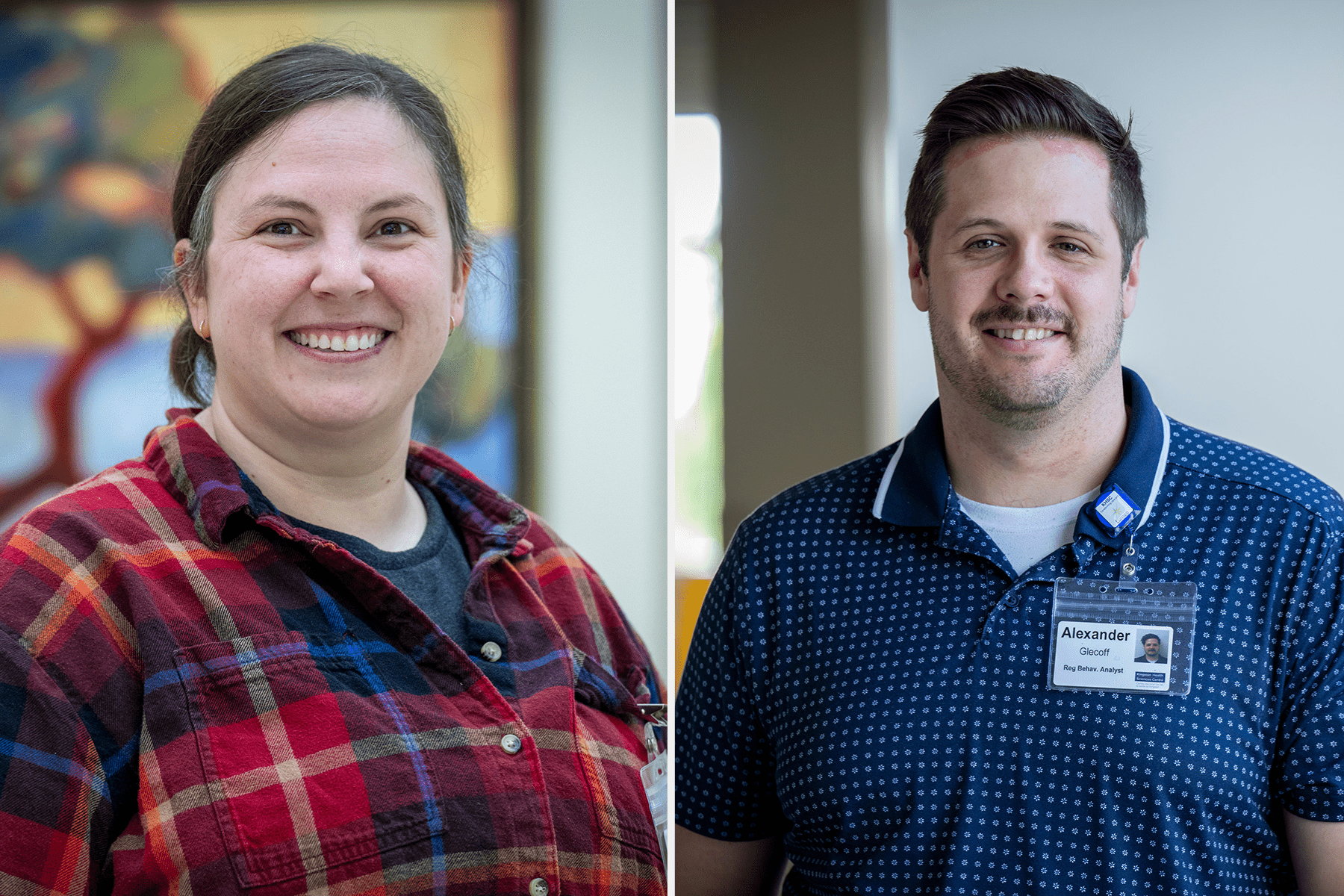
“Think of it like building a bridge,” says Brittany Dolan, who works in the inpatient unit. “My job is to help our team and our patients figure out what’s working and how to keep that going once they’re back home.” She and Alex Glecoff, who works as part of the outpatient program, are the new behaviour analysts at KHSC.
Both analysts work closely with staff and families to develop personalized plans that focus on emotional regulation, social skills, and independent living. It’s a collaborative process involving the entire team of nurses, psychiatrists, social workers, psychotherapists and behaviour specialists working together toward one goal: helping kids move forward with confidence.
Small steps, big progress

“Sometimes, progress is hard to see day by day,” says Dolan. “But when you look back, from when a patient is admitted to when they leave, it can be amazing. You see patients and families come in overwhelmed, unsure how to cope, and by the time they’re discharged, they’re hopeful again.”
And that hope doesn’t stop at the hospital doors. With the right tools, support, and planning in place, families feel more equipped to help their child thrive at home, making this new role a vital part of a family’s journey.
As KHSC continues to face growing demand in youth mental health care, this kind of innovation is more than a nice-to-have. It’s essential.
And it all started with one conversation — and one donor — who believed things could be better.