Effective immediately masking is required for everyone when present on all inpatient units, in the Emergency Department (ED), the Urgent Care Centre (UCC), and the Children’s Outpatient Centre (COPC).

“If it weren’t for the increased need to keep emergency department visits for emergencies during the COVID pandemic, I don’t think I would have experienced the excellent virtual care I received in the comfort of my home after my hospital stay,” says Herbert Rae, a Kingston Ontario resident who, after his emergency gallbladder surgery in May, became the first KHSC patient to be recruited to a study that will test the effectiveness of virtual care and remote monitoring technology on unplanned hospitalizations and emergency visits.
Patients, like Herbert who have been recruited to the study, use simple remote monitoring technology at home to record their vital signs, which are sent instantly to a KHSC nurse. Eleven nurses run the central command centre 24 hours a day, seven days a week. They use tablet computers to visit virtually with patients, including daily assessments for the first 16 days patients are home after their surgeries, and every other day for the remainder of the 30-day enrollment.
Anesthesiologists and General Internal Medicine doctors work on-call to support the initiative and also connect with patients through two-way secure video and texting to address issues that arise day or night.
Not only does the program give patients a feeling of security knowing that their care teams are a click away at any time, it also gives families peace of mind knowing that their loved ones are being closely monitored as if they were in hospital.
“My 87-year-old mom was really happy that I was receiving this level and quality of care after my operation, as the pandemic meant that she wasn’t able to visit me in person and make sure I was doing okay,” says Rae.
“Patients are at highest risk for complications in the first 30 days after surgery, with about 20 per cent returning for emergency care or hospitalization,” says Dr. Joel Parlow, an anesthesiologist who, along with Drs. Kristen Marosi and Ramiro Arellano, is one of KHSC’s principal investigators for the study. “By connecting with patients and helping them seek needed medical treatments early, we can potentially reduce the number of hospital re-admissions and increase our capacity to do more surgeries.”
Approximately half of the KHSC patients recruited to the study will have received technology called Connected Health by Cloud DX, which includes a tablet and remote monitoring equipment to assess six biophysical parameters: blood pressure, heart rate, respiratory rate, oxygen saturation, temperature, and weight. The other half received the current standard care, which is at the discretion of each surgeon and typically includes an in-person clinic visit in two to eight weeks after discharge from the hospital.
Once patients are at home, nurses call them on the phone to set up the equipment. In addition to recording their vital signs at home, patients complete daily surveys that assess their recovery. All data are relayed wirelessly to the nurses who assess it and ensure patients receive the care they need.
“There are so many benefits to a program like this that I can really see this being the way of the future, pandemic or not,” says Tammy Doyle, one the registered nurses providing virtual care. “I believe having patients actively involved in their care in this way will ultimately improve their health outcomes and their relationships with health care providers like me.”
Doyle can recall times when she and the care team were able to manage a patient’s pain remotely, thereby preventing the patient from visiting the emergency department or calling their family doctor. On the flipside, in an emergency, the care team has been able to direct patients to the hospital for life-saving treatment when needed.
“Regardless of patients’ specific recovery experiences, the patients with whom I’ve worked have expressed to me a sense of comfort knowing I was in contact with them regularly and was following their progress,” says Doyle.
A final progress report in the form of a letter is sent to participants’ family doctors to make sure patients continue to be monitored for any issues or concerns that were noted during their involvement in the study.
The study, launched by a team of researchers and health care providers at the Population Health Research Institute of McMaster University, is recruiting 900 adults in Canada who have undergone semi-urgent cancer surgeries, urgent surgeries such as hip fractures, or emergency surgeries such as a ruptured abdominal aortic aneurysm.
Anesthesiology research staff at KHSC has worked to recruit, follow and contribute 200 patients to the 900 total. “I’m very proud of our team’s efforts, which have resulted in KHSC being the number one recruitment site for the project,” says Dr. Parlow. Co-investigators in this multidisciplinary program include three anesthesiologists, three internal medicine specialists, four surgeons and several nurses.
In addition to Kingston Health Sciences Centre, participating hospitals include Hamilton Health Sciences, St. Joseph’s Healthcare Hamilton, London Health Sciences, The Ottawa Hospital and University of Alberta Hospital.
Queen’s Departments of Anesthesiology and Perioperative Medicine, Surgery and Medicine donated funding for the project. KHSC supported the project through the monitoring nurses and providing the monitoring equipment. Seed funding for the trial was also received through Roche Canada’s COVID-19 Innovation Challenge.
“There may be some positive spinoffs of this unfortunate pandemic,” says Dr. Parlow. “There is no doubt that the future of medicine will involve much more care provided remotely, and this project will place KHSC at the forefront of new ways to care for surgical patients.
Gallery



Patient Herbert Rae at home using remote monitoring technology to record vital signs.

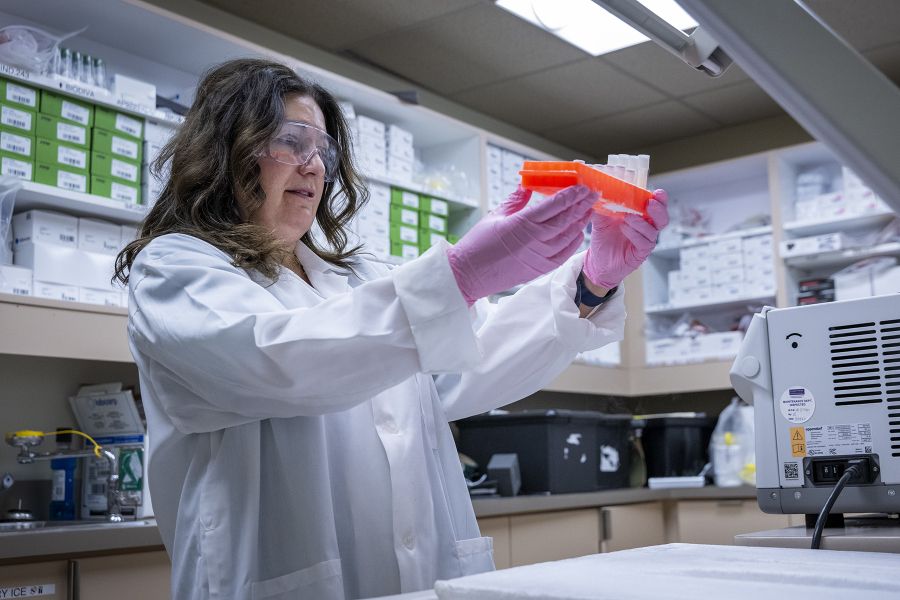
RNs Tammy Doyle and Jenna Paget are among the eleven nurses who run the remote monitoring centre at the KGH site 24 hours a day, seven days a week.