Annual Report 2020-21 - Caring through COVID
COVID-19 made us quicker and more agile at ramping up services. We stood up a super-efficient Assessment Centre, logged a 3000 per cent increase in PCR testing in our Microbiology Lab and added bed capacity by opening a new inpatient surgical unit and creating a temporary alternate health facility. And as the first distributor of the Pfizer-BioNTech vaccine in our region, we launched a much-anticipated vaccine clinic that put more than 25,000 doses of vaccine into the arms of health-care workers across our hospital and community.
Without fail, smart and rapid technological innovation powered us through the pandemic, translating into just over a million electronic screenings for patients, visitors and staff as well as dashboards to manage precious resources and tools to track the infection status of patients. And technology dramatically changed how we connect. Remote work setups are now commonplace, successful and humming with meetings and messages.
Whatever the COVID-19 challenge, patients and families have remained central to our pandemic planning, with family presence policies weighed often and carefully and with strong collaboration with our health care partners to mitigate COVID impacts on the most vulnerable—the homeless and those living with mental health and addiction challenges.
As we wrapped up the year, COVID-19 put us to the biggest test yet as a deadly third wave forced out-of-region hospitals to transfer dozens of COVID patients to KHSC for critical care. We are incredibly grateful to everyone across the organization who responded so swiftly, expertly and compassionately to ensure that our health system had the capacity to care for those who were desperately ill while still maintaining the highest level of care for acute patients in our region.The pandemic remains even as big initiatives come our way in the year ahead: Phase 2 Redevelopment, Accreditation, Health Information System implementation and our new Frontenac, Lennox and Addington Ontario Health Team.
The timeframe of this annual report extends a bit further than usual so that we can tell you the story of our COVID-19 journey over 15 months. Over that time, countless acts of compassion, respect, partnership, excellence and innovation have fortified our workplace culture and established KHSC as a trusted partner and leader in the region and provincial healthcare system. Now, more than ever, we know what we can accomplish together.
Dr. David Pichora
President and CEO, KHSC
David O’Toole
Board Chair, KHSC
Delivering care and capacity
Over the past year, the big challenge for Kingston Health Sciences Centre (KHSC) was balancing COVID-19 preparedness and business as usual. The result was rapid organizational change and new approaches to delivering health care as services were ramped up or down, virtual care strategies deployed, inpatient units repurposed or built from the ground up and more. Wherever the virus turned, we had to ensure that we had the capacity to meet the demands of a regional tertiary care centre and those of a relentless pandemic that strained patients, families and staff alike.
Keeping the virus in check
Staying one step ahead of COVID-19 outbreaks in our hospital and community involved multiple clinical priorities, including the rapid detection of newly infected individuals, assessment centres that could manage hundreds of swabs every day, smart screening tools and infrastructure to administer vaccine when it was finally available. In the face of unprecedented numbers — whether skyrocketing lab tests, around-the-block lineups or thousands of jabs in arms — KHSC excelled at finding solutions and continuously refining them for each successive wave of the pandemic.
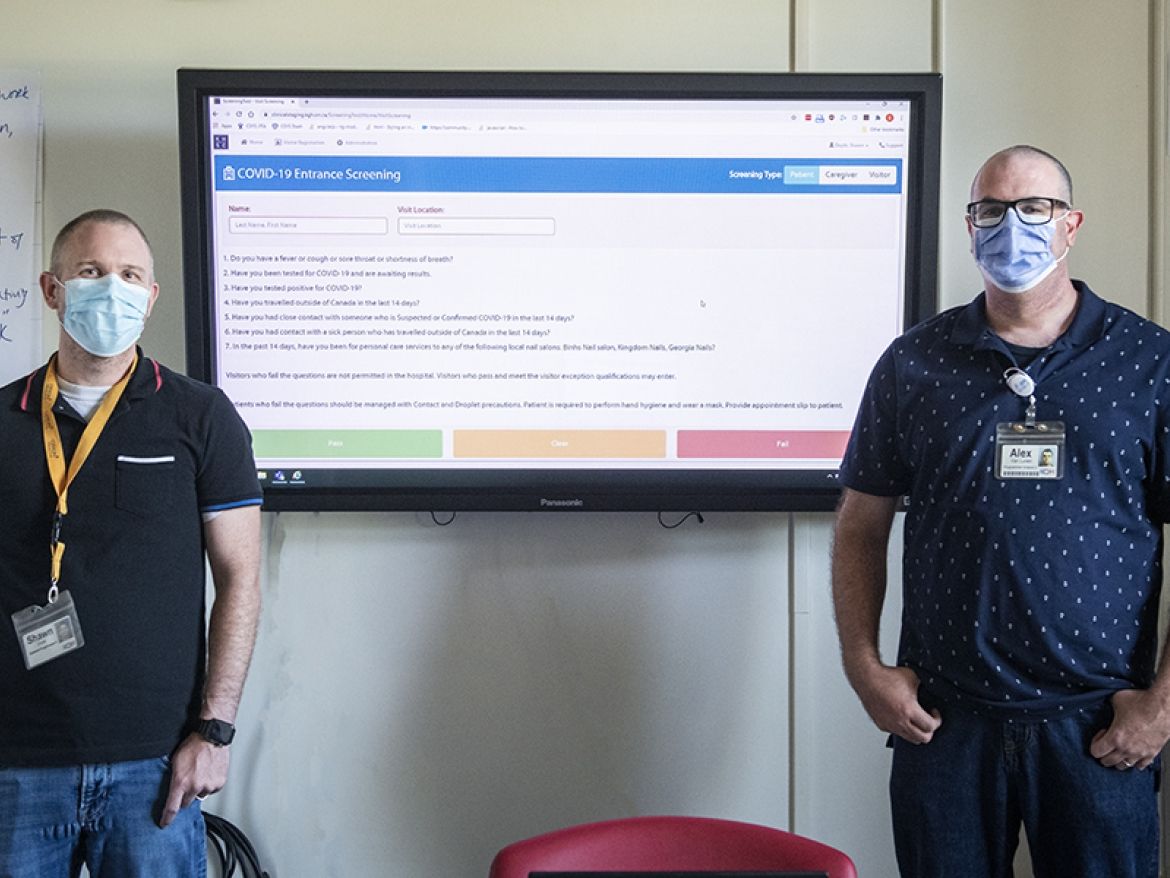
Combating a new virus meant enlisting new communication and decision-making tools at KHSC: dashboards to visually capture the surge in COVID-19 data; real-time flagging of patients’ infection status; entry screening tools; and documentation tools for caregivers permitted to visit loved ones. We also embarked on a remote-work experiment on a scale never seen before at KHSC. COVID-19 relentlessly pushed us to make or accelerate change in our work environment and we responded with speed and innovation.
Practicing bold leadership
Since January 2020, our hospital teams have worked collaboratively and tirelessly to manage COVID-19-related risks at KHSC, including key teams that were on the front lines of staying abreast of COVID-19 science, local prevalence, supply chains, evolving provincial guidance and Public Health recommendations. Translating the intensity and urgency of COVID-19 into policies, practices and protocols that kept our hospital safe — there was not a single case of work-related infection at KHSC — speaks to leadership that was both effective and empowering.
Mobilizing on the research front
Our medical and research community rapidly mobilized to find new ways of tackling COVID-19, with studies ranging from the repurposing of a commonly used medication to treat intubated patients to landing on new ways of mining critical data to investigating virus transmission and immunity among healthcare students and staff. In 2020, for the ninth consecutive year, KHSC was named one of the Top 40 research hospitals in Canada just as everyone was working tirelessly to find creative solutions to the pandemic. “We are very proud of the impact that our clinician scientists are making to translate knowledge into excellent patient care,” says Dr. Steven Smith, VP, Health Sciences Research and President & CEO, KGH Research Institute. “Our research is transforming patient care for today and for the future.”
2020-2021: By the numbers
Fiscal 2020-2021 brought an onslaught of changes and challenges to KHSC. Our teams responded, innovated and excelled. The impressive numbers tell the story.
We invite you to stay connected with us so you can keep track of the exciting things happening at Kingston Health Sciences Centre. Read all of our most recent news on our website or engage with us on social media by following our accounts on Twitter and Facebook.
If you would like to ask us a question or share a comment, simply click here.
Long Image Text
<p>Virtual care at KHSC was once rare, although just prior to the pandemic a successful pilot project tested virtual follow-up visits for stroke care. During the first wave of COVID-19 KHSC jumped to deploy the Reacts platform as a way to conduct urgent visits that did not need require an in-person visit. In their first month, video visits, in some cases, went from zero to 30 per cent. In 2020-2021, the number of health-care providers using virtual care increased to over 800, with almost 145,000 visits conducted by phone and 40,000 by video, giving patients access to appropriate care in the comfort of their homes.</p>
Long Image Text
<p>As part of the government’s COVID-19 preparedness plan, we opened a new inpatient surgical unit at our Hotel Dieu Hospital site and expanded the site’s Extended Post-Anesthesia Care Unit. With more than 40 new surgical beds, KHSC was able to continue scheduled short-stay surgeries that may not have otherwise happened if bed availability had been curtailed. Along with improving patient access to surgical care, the extra beds helped KHSC to address a long-standing challenge of having the right number of beds at the right time to manage the increasing demand for acute inpatient care.</p>
Long Image Text
<p>Faced with a potential surge in COVID-19 patients, we stood up a satellite site to serve as a relief valve for our two hospital sites and to support non-COVID, medically stable patients. Working with community partners over mere months, we retrofitted and equipped part of a decommissioned local hospital to create 70 beds at the temporary Union Street site. It was an all-hands-on-deck effort that demanded a fast, agile response from more than a dozen patient care, planning and support teams. Together, they built a safety net of staffing, supplies and equipment that, ironically, they hoped circumstances would never force them to activate.</p>
Long Image Text
<p>As COVID’s third wave ran rampant, KHSC stepped up to accept critically ill COVID patients from elsewhere in the province who were very sick and mostly ventilated. While land and air transfers were not a new phenomenon, the scale this time was unprecedented. We bumped our ICU bed capacity from 65 to 95, while ramping down elective surgeries and less urgent care so staff could be redeployed and resources focused on the surge of patients. At the same time, we worked closely with our regional health care partners to transfer appropriate patients in order to free up capacity at KHSC to provide complex, acute and critical care.</p>
Long Image Text
<p>During the third wave of the pandemic we focused on ensuring critical care beds and the staff to support them as severely ill patients were transferred to KHSC from elsewhere in the province. More than 200 staff were retrained and redeployed, including nurses, allied health professionals and administrative staff. Learners were on boarded for assistant roles in nursing, physiotherapy and occupational health, with an eye to the support and rehabilitation that recovering COVID patients would need before discharge. And physicians from all medical specialties worked around the clock, sometimes in care settings new to them, to provide care.</p>
Long Image Text
<p>A son, a father and a husband, Lewellyn Allworth was transferred to our ICU from the Greater Toronto Area on a ventilator. While he doesn’t remember much of his first few days at KHSC, he was left with a clear impression of how much the staff cared for him and other patients. “The people here became my family,” he says. “They saved my life. It’s the only place I’ve ever seen this level of teamwork and camaraderie. Everyone seems like they love what they do and were all so kind to me. The Kingston community should be very proud of this hospital.”</p>
Long Image Text
<p>Temporary restrictions to family presence challenged our usual approach to patient and family-centred care and were a source of upset for patients, families and staff alike. Regular and robust consultation with patient and family advisors was key to helping us proactively adjust family presence. Finding alternatives to usual family presence was necessary, including linking patients, families and clinicians by phone to discuss treatment and launching a new Staying Connected program that made virtual visiting possible. In the pandemic environment, these strategies went a long way towards helping with collaborative decision-making and participation in care.</p>
Default Title for Slide
Default Title for Slide
Default Title for Slide
Default Title for Slide
Default Title for Slide
Default Title for Slide
Default Title for Slide
Long Image Text
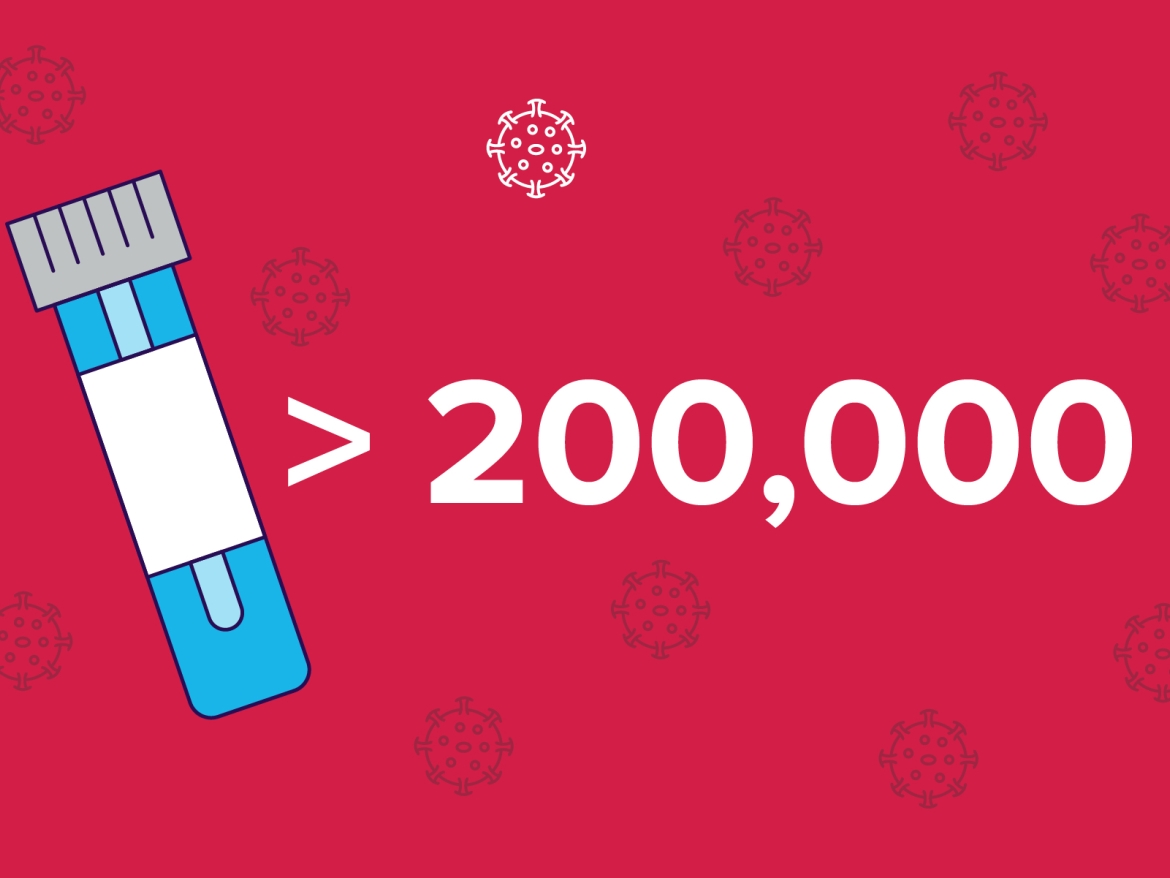
<p>Our Microbiology Lab played a critical role in regional testing. Since coding the COVID-19 test in record time in March 2020, the lab team has tested more than 200,000 samples from across southeastern Ontario — 40 times more than a typical year. Even with the massive workload, the lab was consistently a leader in turnaround times and was selected as one of the few genomic sequencing sites to identify and manage COVID-19 variants in the province. Even so, the testing has felt like business as usual. “It's no different from running any high volume test,” remarks Rebecca Kooi, a medical lab technologist. “Every sample we run has a patient behind it, and the results have an impact on that person.”</p>
Long Image Text
<p>KHSC scrambled to open Kingston’s first Assessment Centre (AC) in less than a week in March 2020. As the demand for testing grew, the Centre relocated three more times in the next year, always supported by strong community partners. It weathered heat waves, pop-up sites, long line-ups and outbreaks that could send swabs skyrocketing to 700 per day. In March 2021, the AC marked a one-year total of more than 80,000 tests. Every step of the way the AC team was committed to making the experience as positive as possible, going through thousands of lollipops, stickers and finger puppets to ease the stress for patients and families.</p>
Long Image Text
<p>The first Pfizer-BioNTech COVID-19 vaccine dispenser in southeastern Ontario, KHSC worked in partnership with Public Health (PH) agencies in early 2021 to vaccinate about 1,700 health-care workers and essential caregivers in long-term care and high-risk retirement homes throughout the region. KHSC also supported the work of PH mobile vaccination teams to vaccinate the residents of care homes to decrease the risk of deadly COVID-19 outbreaks in those vulnerable settings. And by April 1, 2021, we had put the first dose of vaccine into the arms of almost 6000 KHSC employees.</p>
Long Image Text
<p>When people picture a team of healthcare workers during a pandemic, it likely doesn't include electricians, carpenters and plumbers. But those teams were essential in keeping our sites safe and operational. Carpenter David De Sousa likens his team to one of many branches on a tree. "Our roots provide a strong trunk, and all the people who work here are the branches. If you remove some branches the tree can suffer but together we thrive." Since March 2020, he has been churning out endless plexiglass barriers. "Now people want to keep the screens year round,” he says. “If I had known, I would have started building them earlier!"</p>
Default Title for Slide
Default Title for Slide
Default Title for Slide
Default Title for Slide
Long Image Text
<p>Thanks to an incredibly strong Decision Support team, we hit the ground running in the early days of the pandemic to produce the situation dashboards needed to track beds, staff, ventilators and personal protective equipment (PPE). Decision Support boosted its efficiency in mining new data pipelines and building automatic processes for pulling that data. The dashboards — along with others created, for example, to manage allocation of surgical cases or to identify patients by “hot” Public Health Unit zones — were vital to decision-making about patient flow, PPE stewardship, infection control measures and more.</p>
Long Image Text
<p>The job of tracking the infection status of admitted patients has never been more critical. COVID-19 prompted us to revamp our process for flagging patients who require infection control precautions, further streamlining and automating it to produce real-time electronic flagging when a patient requires precautions. The alert also aims to ensure that everyone on the patient care team — from physician to porter — can access a patient’s infection status from doorway to discharge. Strengthening and expanding the flagging process only reinforces the fact that infection control is always a team effort at KHSC.</p>
Long Image Text
<p>COVID-19 ushered in a new world of remote work at KHSC. Information Management (IM) launched remote access technologies almost overnight in March 2020 with a SWAT team swinging into action to handle up to 40 requests per day for remote work station set-ups. Now, about 700 employees have access to a seamless computer experience between work and home. At the same time, IM accelerated a planned roll-out of the Microsoft Teams virtual meeting tool. The remote work model has broadened our thinking about its potential as we look at decanting of staff and space for KHSC’s upcoming Phase 2 Redevelopment Project.</p>
Long Image Text
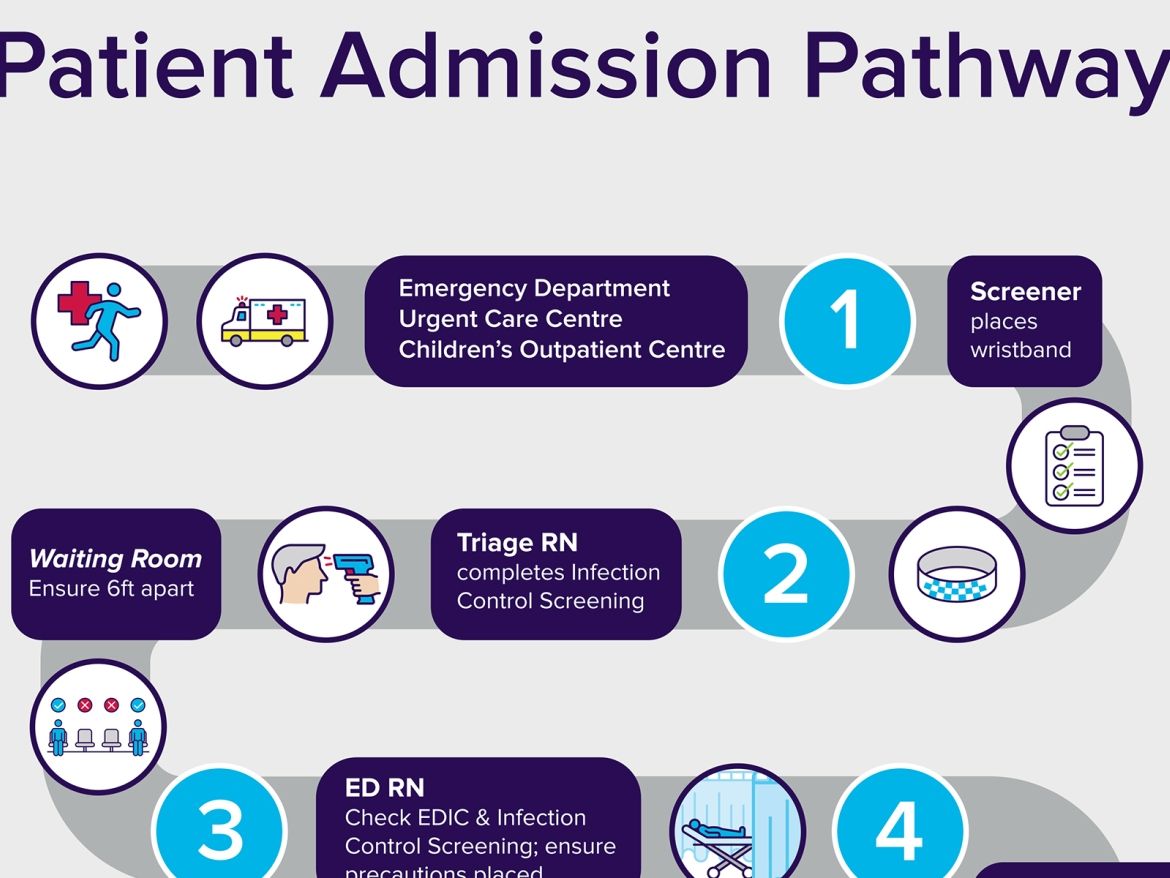
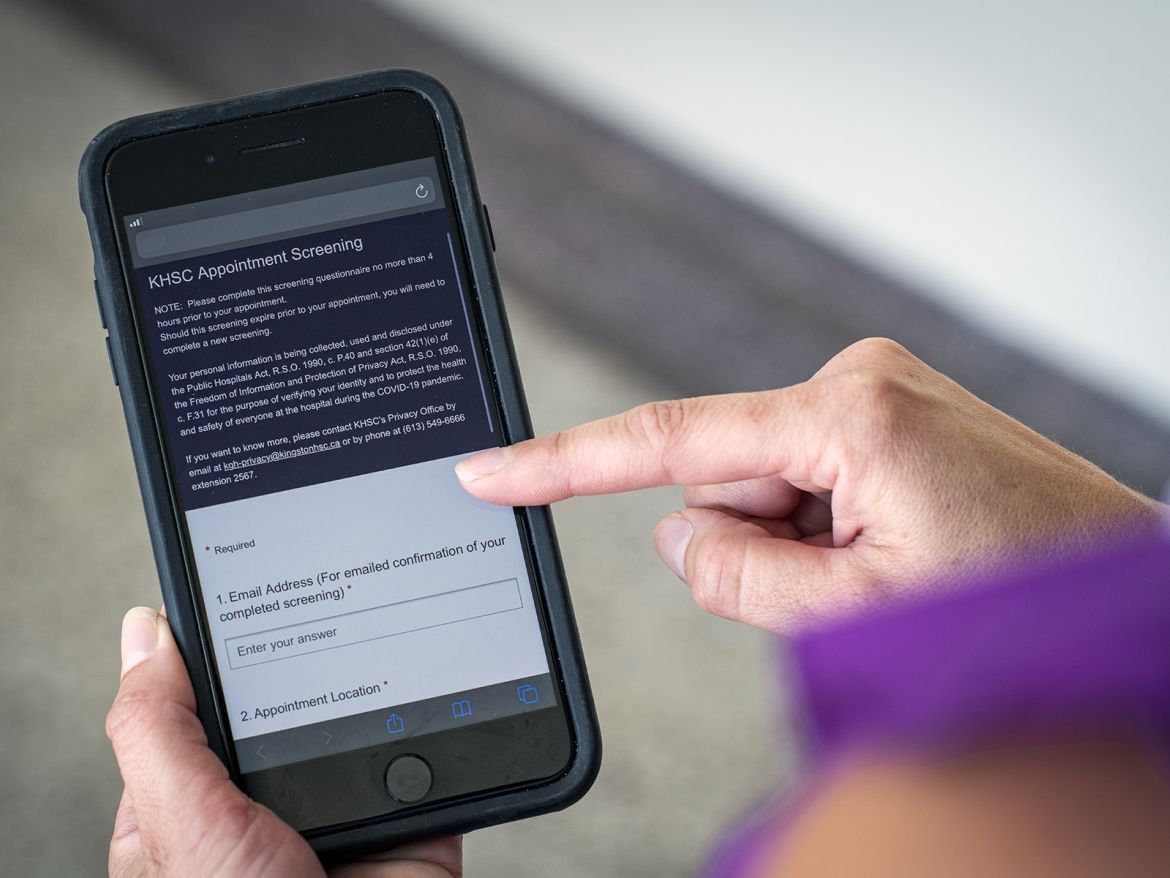
<p>Smart screening tools played a major role in keeping the virus at bay. For staff — who logged more than a million screenings in 2020 — the big logistical challenge was getting hundreds of people through screening quickly. The answer was a custom-built tool with an algorithm that instantly identified people who may be a risk. As the screening protocol changed, the software did likewise. To support more efficient flow for outpatients, we built a mobile pre-screening tool that let patients complete their screening prior to arriving at the hospital. With input from our patient advisors, the tool exemplified partnership and innovation at KHSC.</p>
Long Image Text
<p>With family presence strictly limited, we needed a safe and seamless solution for documenting essential care partners for patients. On cue, our information and project management teams built, tested and launched a web-based tool that lets hospital staff register family members approved to visit or accompany a loved one. And the tool makes it easier to do contract tracing. We know how crucial care partners can be to loved ones in hospital, which made landing the visitor registration tool a priority. It creates the right balance between ensuring patient and family-centred care and protecting the safety of all those in our hospital.</p>
Default Title for Slide
Default Title for Slide
Default Title for Slide
Default Title for Slide
Default Title for Slide
Long Image Text
<p>Navigating the uncharted waters of COVID-19 called for a steady hand at the helm. That hand was Incident Command, a core group of leaders with the collective organizational expertise to ask — and answer — the right questions about safety, capacity, infection control, staffing, testing, supply chain and more. Over 14 months, it acted upon countless directives, dashboards and briefing notes to develop optimal solutions in real time. Always, it made transparency a priority: “We created a discipline of telling people here is what we know and don’t know. It was clear that we performed better when people had as much clarity as possible,” says now-retired Incident Commander Troy Jones.</p>
Long Image Text
<p>Our Infection Prevention & Control (IPAC) team set a relentless pace in adapting and implementing rigorous protocols around PPE, precautions, contact tracing and infection tracking. In the middle of the pandemic, they implemented a custom software solution to complete whole-house infection surveillance; streamlined electronic flagging and documentation of a patient’s infection status from doorway to discharge; created a new outbreak management toolkit; and developed a critical IPAC safety playbook. The team’s unswerving leadership was absolutely key in managing risk, which was critical in minimizing anxiety for patients and staff alike.</p>
Long Image Text
<p>As the science of COVID-19 rapidly evolved, our Occupational Health, Safety & Wellness (OHSW) team was challenged every day to protect our workplace. Undaunted, they constantly revised safety guidelines; assessed masks, gloves, sanitizer and other personal protective equipment; fit tested 5,000 N95 respirators; reworked screening questions; conducted contact tracing and swabbing; and helped to prioritize health care workers for vaccine. “And anxiety resulted in huge influxes of staff calls,” says OHSW Leader Beth Spratt. “We provided a lot of emotional support, conscious that staff were dealing with COVID-19 at home as well as in the workplace."</p>
Long Image Text
<p>He has become one of the most sought-after and reassuring voices in the world of COVID-19. As KHSC medical director of infection prevention and control, Dr. Gerald Evans has spent the last year protecting patients and staff amidst a swirl of protocols and practices. He kept his balance by staying current with the fast and furious medical science of COVID-19: “I worked really hard at keeping everyone calm and not being fearful of what seems scarily unknown.” In the face of dire stats or projections, he stuck to what wins the day: evidence-based solutions, good teamwork and common sense. His biggest COVID takeaway? “Never losing sight of all the good people and good work happening around me.”</p>
Default Title for Slide
Default Title for Slide
Default Title for Slide
Default Title for Slide
Long Image Text
<p>During the first wave of the pandemic, Herbert Rae became the first KHSC patient to be recruited to a national study to test the effectiveness of using technology to remotely monitor patients after surgery. Approximately 200 KHSC patients made up the 900 adults in Canada who participated in the study. Connecting regularly with surgical patients during the 30 days after they’ve returned home, holds the possibility of helping patients seek needed medical treatments early and potentially reducing the number of hospital re-admissions. This research has developed into an important pilot project at KHSC to expand this type of virtual care to more surgical patients.</p>
Long Image Text
<p>At just the right time, the Accelerated Remote Consultation Tele-POCUS in Cardiopulmonary Assessment (ARCTICA) research project is helping to provide life-saving tools and training in point-of-care ultrasound for physicians working in remote healthcare locations. “Point of care ultrasound is a powerful tool for assessment in people who have shortness of breath,” says KGHRI researcher Dr. Amer Johri. “But while ultrasound is available even in remote areas of Canada, many physicians lack the opportunity to develop expertise in this potentially life-saving skill.” The project uses real-time remotely supervised ultrasound consultations and education modules to provide training and support for cardiopulmonary assessments.</p>
Long Image Text
<p>The COVID-19 pandemic is a societal stressor that has overwhelmingly increased the demand for mental health care. Dr. Nazanin Alavi, a psychiatrist at KHSC was among 13 recipients of Queen’s University’s Rapid Response funding competition supporting COVID-19 research. Through this research, nine weeks of online cognitive behavioural therapy (CBT) is offered to help people manage the burden and stress caused or increased by the pandemic. The CBT modules are focused on coping skills and resilience building, which have been shown to be effective in the treatment of mood and anxiety disorders, and ultimately improving quality of life.</p>
Long Image Text
<p>KGHRI researcher Dr. Steven Brooks has teamed up with colleagues across the country to develop a new emergency department (ED) network that uses big data to improve patient care. The Canadian Emergency Department Rapid Response Network is a 51-site, pan-Canadian network of EDs building a registry of suspected and confirmed COVID-19 ED patients. By collecting detailed information about the patients, the network aims to better understand and test clinical processes, and monitor patient outcomes once they return home. The network is receiving in-kind support from partnering hospitals, as well as funding from the Canadian Institutes of Health Research and the Government of Ontario.</p>
Long Image Text
<p>KGHRI researchers Drs. Anne Ellis, Stephen Vanner and Prameet Sheth received over $200,000 in federal funding to advance research that examines SARS-CoV-2 transmission and immunity among students and staff in clinical placements, with a goal of testing for SARS-CoV-2 and monitoring the seroprevalence of health professional students at Queen’s University. The study is recruiting 500 asymptomatic students from the Faculty of Health Sciences who routinely interact with each other, the public and ambulatory and inpatient populations. Researchers test the students for active COVID-19 infection and virus antibodies. The results are expected to help shape pandemic management policies and procedures.</p>
Default Title for Slide
Default Title for Slide
Default Title for Slide
Default Title for Slide
Default Title for Slide
Long Image Text
<p>Our MIcrobiology Lab tested more than 200,000 samples for COVID-19 over the last year. Typically, in previous years, we did about 5500 PCR tests annually. The pandemic boosted us to 40 times more or a 3,000 per cent increase.</p>
Long Image Text
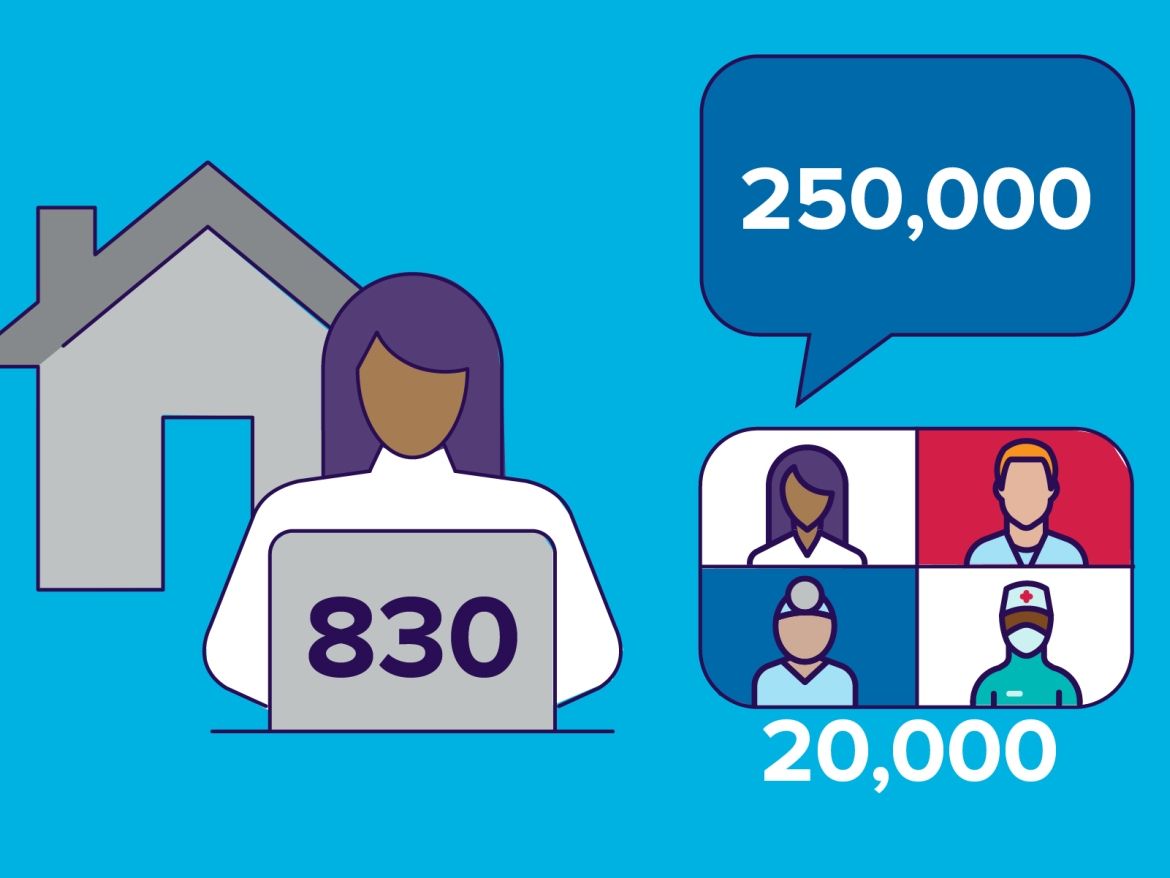
<p>Remote work setups are now more commonplace for KHSC employees. Every day, 830 people log onto Microsoft Teams. In the last 90 days alone there have been approximately 20,000 meetings and 250,000 chat messages.</p>
Long Image Text
<p>It takes a lot of hands to tackle a pandemic. To meet the challenge, we hired over 900 new employees. And recruiting continues!</p>
Long Image Text
<p>In a matter of months we worked with community partners to transform off-site decommissioned hospital space into the 70-bed Union Street site, an alternate health care facility ready to hand in the event of surging patient volumes due to COVID-19.</p>
Long Image Text
<p>Our clinical engineering team deployed 400 medical devices to support our temporary Union Street site, along with our main site COVID-19 unit, Intensive Care Unit and inpatient surgical expansion.</p>
Long Image Text
<p>Everyone who enters our buildings must complete strict COVID-19 screening. There have been close to 1.7 million total electronic screening transactions including those for patients, visitors, caregivers and staff.</p>
Long Image Text
<p>As the first distributor of the Pfizer-BioNTech vaccine in the South East, we set up a KHSC vaccination clinic to get thousands of doses of vaccine into the arms of health-care workers in long-term care and high-risk retirement homes, and in the community and hospitals. So far, we have administered over 25,000 doses.</p>
Long Image Text
<p>Our Sprinkle Some Joy campaign has been a bright spot this year, as a grateful community said thank-you to KHSC staff through the donation of 50,000 gifts including gift cards, meal vouchers, sweets and beverages.</p>
Long Image Text
<p>We opened a new inpatient surgical unit at our HDH site, bringing 40 new surgical beds online so we could continue to perform scheduled surgeries, minimize further backlogs and also address a longtime challenge of having the right number of beds at the right time.</p>
Long Image Text
<p>Our Community Assessment Centre team stood up four different locations over the year and has taken more than 115,000 test swabs, always bringing a warm smile, care and compassion to anxious members of our community.</p>
Default Title for Slide
Default Title for Slide
Default Title for Slide
Default Title for Slide
Default Title for Slide
Default Title for Slide
Default Title for Slide
Default Title for Slide
Default Title for Slide
Default Title for Slide
We will not soon forget the year 2020-2021. As much as we would like to wish the year away, we can take pride in the fact that it made us stronger and more resilient. The virus was tough but we were tougher.