When John More woke up on March 3, 2025, something was wrong. He could move around, but suddenly struggled to find the right words. What began as a quiet morning at home in Napanee turned into a months-long journey of recovery.
“I got out of bed, couldn’t communicate with my wife, and she called 911. I couldn’t move, had difficulty understanding things, and it was hard for me to speak.”
The ambulance took John to Lennox and Addington County General Hospital in Napanee , where staff suspected a stroke but needed additional tests. He was transferred to Kingston Health Sciences Centre (KHSC), the region’s tertiary care centre. After several hours of diagnostics, doctors confirmed he’d had a stroke, though his condition was stable. He was discharged after several days for close monitoring.
Strokes can be difficult to diagnose. Some appear instantly and progress quickly, while others develop more subtly, carrying the risk of escalation over time. Each case is unique.
Six weeks later, John was back at KHSC.
“My speech problems got worse, so I went back to the hospital. They told me my carotid artery was blocked and my only option was to basically redo everything in my neck.”
An urgent endarterectomy — a surgical procedure to clear the blockage — was needed.
“They told me if they couldn’t finish within two minutes, I wouldn’t make it. Thankfully they did,” he recalls.
After four days of recovery at KHSC, John was transferred to Providence Care, where he began his rehabilitation on the stroke unit of Providence Care Hospital. His focus: overcoming aphasia — difficulty recalling words and speaking.
“After about three weeks, I was discharged to Providence Care’s Outpatient Stroke Rehabilitation program. I had 12 weeks of outpatient therapy — speech, OT, and PT. I drove from Napanee every day.”
Recovery and resilience
Now enjoying his third retirement, John approached recovery with focus and discipline.
“If there’s one thing I’d recommend, it’s to make sure you do physical therapy, even if you feel fine. I didn’t really have any physical symptoms but, for me, it gave me tangible goals I could track. It gave me goals and motivation which was mentally helpful. It balanced the more challenging cognitive therapy I had with speech and occupational therapy.”
He credits his therapy team for providing personalized exercises and encouragement — routines he continues to this day.
“Now, I can function in the community, talk to neighbors. Sometimes I stumble, but that may improve with time. I try to stay optimistic and keep working at it.”
Innovative tools for recovery
Always an innovative thinker, John turned to AI as a tool in his recovery.
“I started using AI early on, even as an inpatient. I had a lot of trouble speaking and didn’t really understand what was going on, so I brought my laptop and could use prompts to help understand what exactly happened to me.”
As he progressed, he used AI to tailor his own comprehension exercises.
“A lot of the exercises didn’t relate to me, so I used AI to generate tailored materials for comprehension. It was a natural evolution.”
Strengthening stroke care through innovation
Behind every stroke case is the Regional Stroke Network — a collaboration of hospitals ensuring patients get the right care at the right time. Clear, consistent information is critical. Patients often move quickly between sites, and their information must move with them.
That’s why new tools like Lumeo, the region’s new health information system, are so important. With digital charting, care teams can instantly access accurate, up-to-date patient information across sites — from medications to therapy notes — improving communication and reducing duplication.
For Dr. Albert Jin, medical director for the Regional Stroke Network of Southeastern Ontario, the consistent, immediate exchange of information is crucial:
“Lumeo has been very helpful for information gathering in critical care situations like stroke, where every minute we can save in getting the right information translates to quicker care and better outcomes for the patient.”
For John, tests done in Napanee were immediately available at KHSC and later at Providence Care, ensuring seamless continuity of care.
“The implementation of Lumeo has kept John’s care connected across hospitals and outpatient rehab,” says Sheryl Gibson, Providence Care Manager, Rehabilitation Services. "This means physicians, nurses and allied health staff like physiotherapy, speech language pathology and occupational therapy, have the same up-to-date information, keeping care coordinated and wellness on track.”
That kind of integration is the foundation for modern healthcare — a journey that continues with research projects like one led by Dr. Siddhartha Srivastava, exploring how generative AI can reduce administrative burdens for providers. Funding for the AI research project was made possible by the Canadian Medical Association, MD Financial Management Inc. and Scotiabank as part of the Health Care Unburdened Grant program.
A system working together
John’s story is a testament to what’s possible when teams, technology, and determination come together. From the rapid coordination of stroke care to the innovative use of digital tools and AI, his journey reflects how collaboration across KHSC, and partner healthcare providers is helping patients recover faster, regain independence, and return to the lives they love.
Gallery



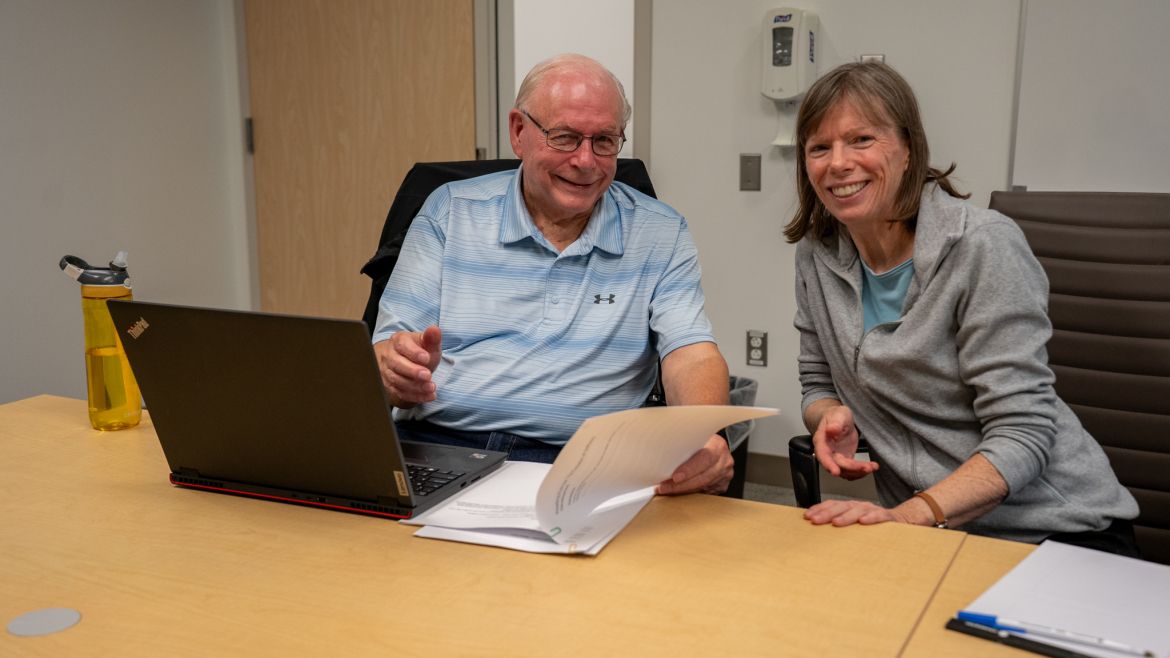
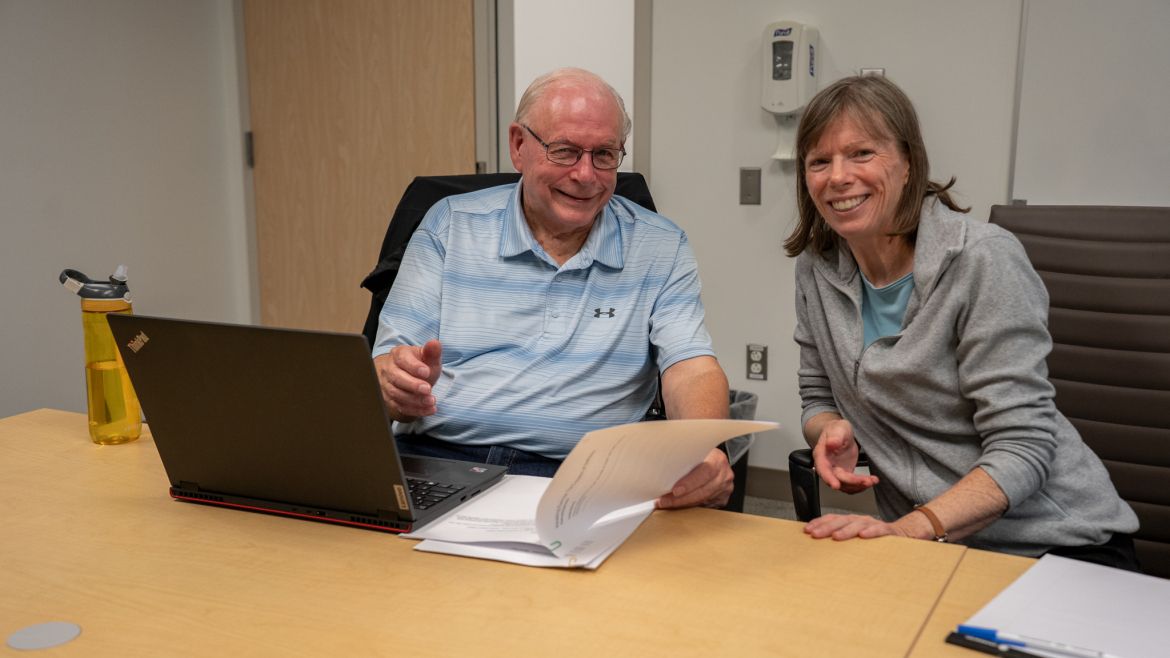
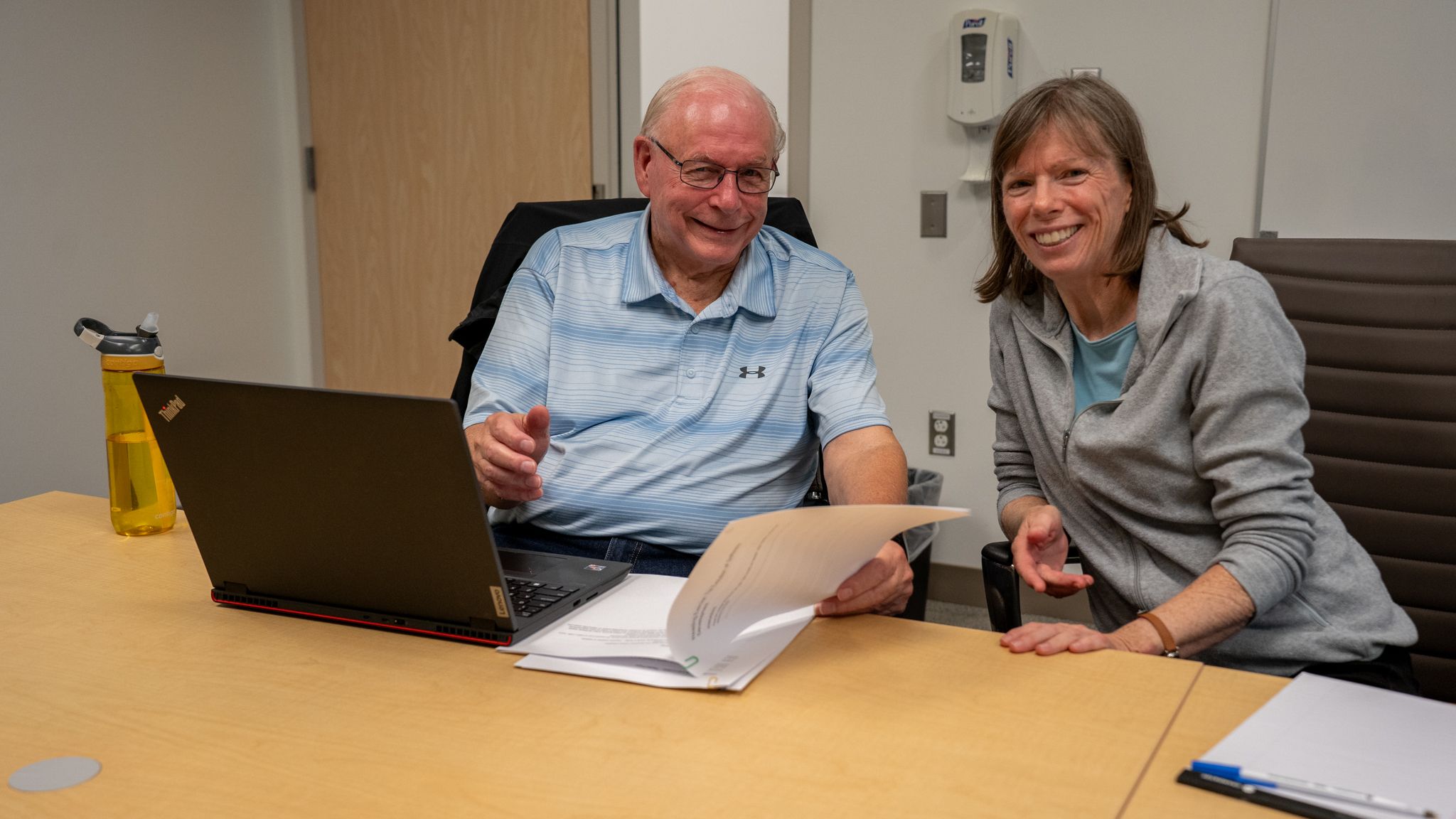
Patient John More and Speech Language Pathologist Theresa Whalen