
Dr. Bob Connelly isn’t usually on the receiving end of care at Kingston Health Sciences Centre (KHSC). As the medical director of the pediatrics program, he usually spends his days caring for KHSC’s youngest patients.
After finding out he needed surgery and waiting nine months for a total hip replacement surgery, in April, Dr. Connelly got to experience the surgical program’s process improvements firsthand.
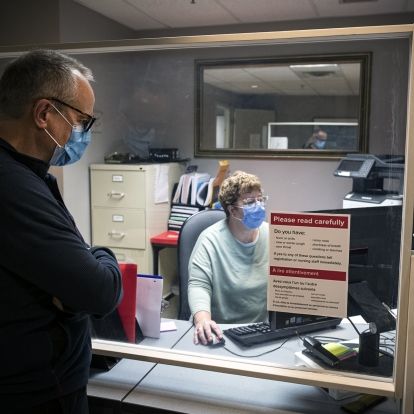
He arrived at KHSC’s Hotel Dieu Hospital site’s day surgery unit at 6 a.m. and by 5 p.m. the same day he was back home.
While that doesn’t seem like a lot of time to be in the hospital to get a new hip joint, Dr. Connelly says he was well prepared for his surgery and felt very ready to leave the hospital and return home.
“The first piece of education I received was the patient booklet, which was thorough and easy to understand. Receiving it early on was helpful and meant I was able to ask questions during my pre-surgical screening appointment several weeks before my surgery.
“I also decided to use the SeamlessMD digital care platform and that made it easier to find the information I needed about my surgery. I liked how it gave me a countdown to my surgery date, helping me focus on my preparations. After my surgery, I continued to refer to it and used it to do things like track my use of pain medication and snap a picture of my incision site when I had questions about how red it was.
“My one-on-one visit with the physiotherapist before my surgery was also very informative, teaching me the exercises I would do after my surgery and answering all the questions I had about the equipment I would need to use to support my recovery.”
Physiotherapist Melissa Magtanong explains that changing from group education classes to individualized appointments one to two weeks prior to surgery has made it possible to eliminate or minimize the traditional in-hospital physiotherapy visit after surgery. “Patients can go home, having already received all the information they need, including a referral to a physiotherapist in the community.”
“I simply cannot say enough about the staff, my surgeon Dr. Mann and my anesthetist Dr. Sydor. They were incredible at answering my questions, being attentive to my needs and being very compassionate,” says Dr. Connelly.
In addition to enhanced patient preparation and education, several other improvements have been made throughout the patient journey to help cut the length of stay for same-day hip and knee replacement patients by almost half, including changing the drugs and doses used to temporarily stop the sense of pain during procedures.
Transforming care, together
The surgical program at KHSC is no stranger to continuous improvement. With limited physical and health human resources, and long waitlists that existed even before the pandemic, team members are familiar with asking themselves what can be done differently to better serve patients.
For a long time now, KHSC anesthesiologists have been delivering local pain-blocking and numbing medicine (anesthesia) through shots in and around the spine. This approach improves patients’ recovery after joint replacement surgery compared with general anesthesia which makes patients totally unconscious and from which it takes longer to wake up.
To improve the use of spinal anesthesia, Dr. Yuri Koumpan says anesthesiologists have been using new local anesthetics and fine-tuning the amounts given, with the goal of getting patients moving within hours of finishing surgery. They are also using a variety of different medications before, during and after surgery to target pain, nausea and vomiting.
“Together with the surgeons, nurses and physiotherapists, we’ve been successful in improving patient outcomes and helping patients go home sooner – many go home the same day of surgery,” says Dr. Koumpan.
Even before the pandemic, orthopedic surgeon Dr. Steve Mann says the surgical program was working on getting more patients home on the day of surgery, as there is growing evidence this is safe, preferred by many patients and is resource-effective for hospitals.
“COVID put all of that work on hold for about three years, during which time we did less than 50 per cent of our regular volume of hip and knee replacements, but we’re getting close to being back up to pre-pandemic volumes for these surgeries,” says Dr. Mann.
Recently there has been a lot of work done to deliver spinal anesthetics and nerve blocks outside the actual OR. Dr. Mann believes this has improved efficiency and decreased the stress about completing a full slate of cases on time. “This new process allows the anesthetic time to run at the same time as the previous case is finishing and the room is being cleaned and set up for the next case, rather than the spinal happening in the OR while everyone else waits.”
Slow, steady progress
While it is not unusual for people to wait longer than the target wait times set by Ontario Health for non-emergency surgeries, it is unusual for the list of “over-target waiters” to make up more than half of KHSC’s overall surgical waitlist, which is what has happened as a result of years of provincial surgical ramp downs during multiple COVID-19 hospitalization surges and ongoing staffing challenges.
Hip and knee replacements and cataract surgeries are a couple of examples of the types of procedures that have been most affected by pandemic-caused delays. They also make up the majority of the over-target waiters waitlist.
Since April 2022, through process improvements, KHSC has managed to reduce the number of patients waiting longer than targeted timeframes for less-urgent surgeries by six per cent and has reduced its total surgical waitlist by approximately eight per cent.
Gallery
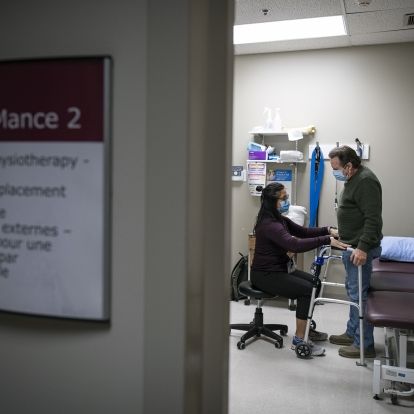





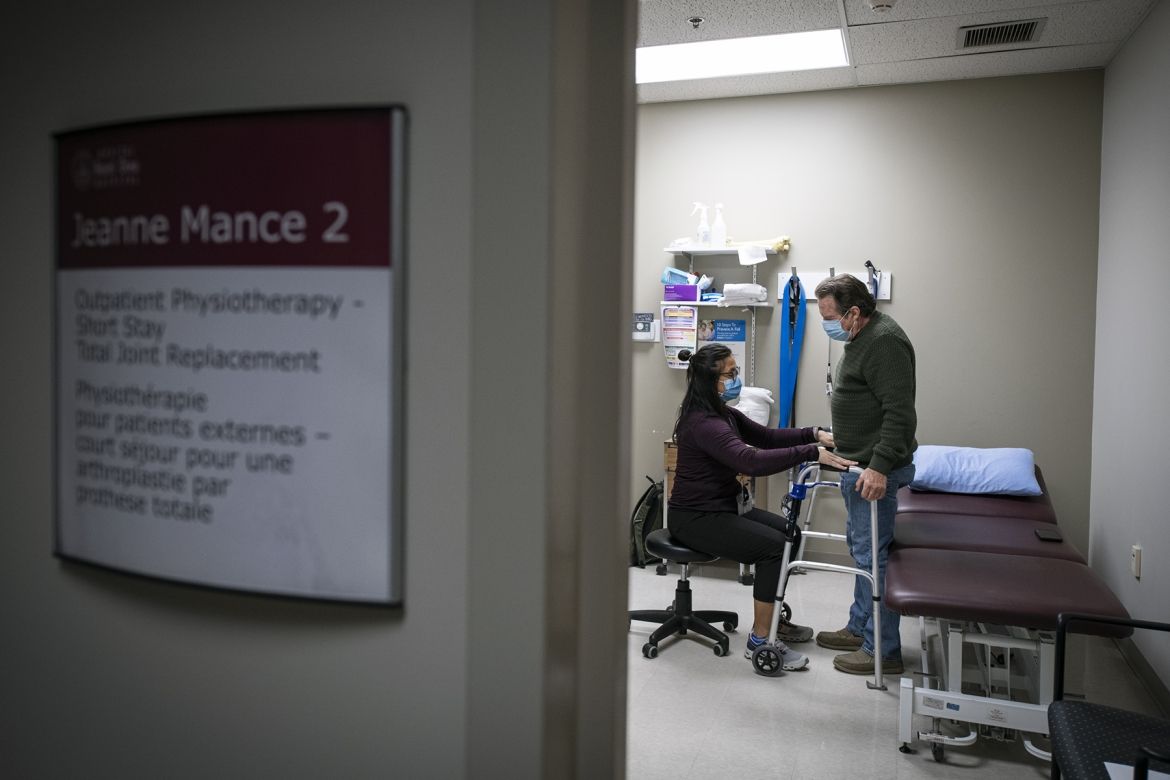
Physiotherapist Melissa Magtanong with a patient during a pre-surgical appointment.
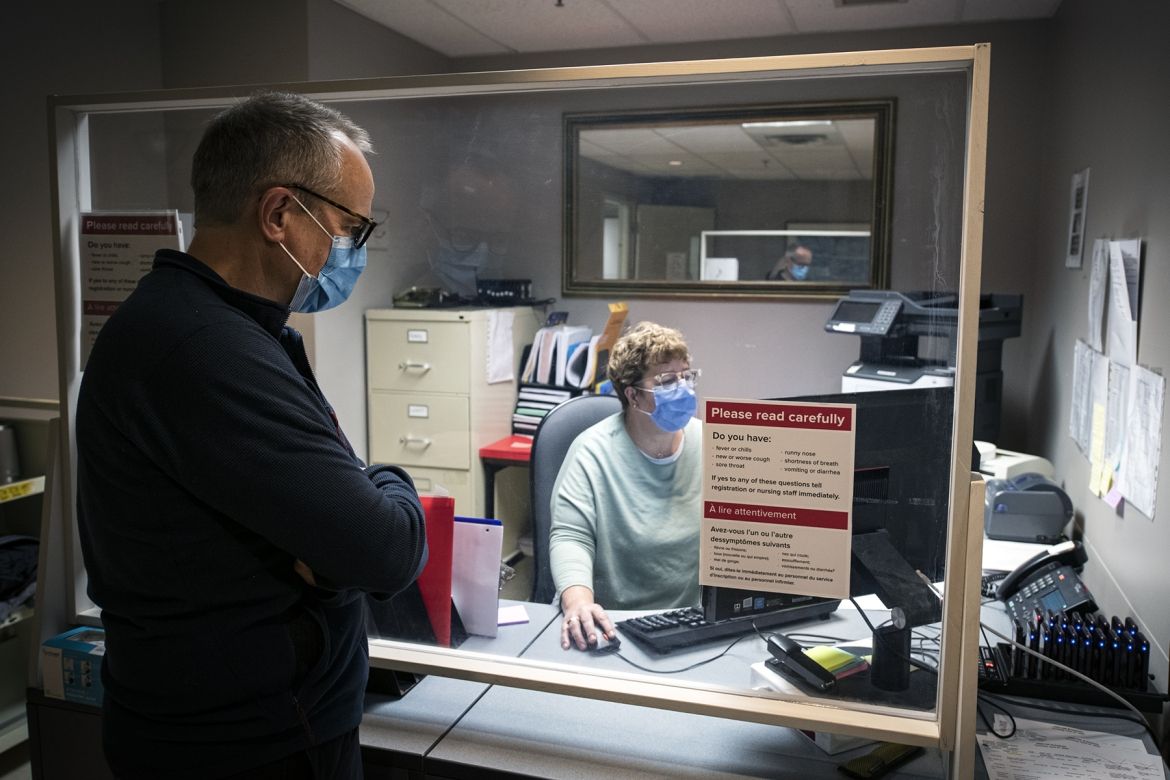
Dr. Connelly checks in at the HDH site's Day Surgery Unit (JM2) at 6 a.m.

Dr. Connelly receives spinal anesthesia.

Nurses in Post-anesthesia Care Unit with Dr. Connelly.

Orthopedic surgeon Dr. Steve Mann speaks with Dr. Connelly after surgery.

Dr. Connelly speaks with a nurse after surgery about how he is doing and when he will be able to go home.

Health Literacy Team nurses (left to right) Dianne Breen, Amy Ronan, and Stacey Cox with Alex MacKinnon, interim manager of Clinical Resources and Transitional Care. Using SeamlessMD, nurses monitor patients' progress virtually after surgery.



