Effective immediately masking is required for everyone when present on all inpatient units, in the Emergency Department (ED), the Urgent Care Centre (UCC), and the Children’s Outpatient Centre (COPC).

A key success factor in helping people manage disease is time: taking the time to understand patients’ unique symptoms, explaining what activities to avoid, and providing plenty of opportunities for questions to be answered. Time is what Kingston Health Sciences Centre’s (KHSC) COPD Nurse Navigator Kim Spearing gives her patients, as she educates them on how to recognize when their usual symptoms are getting worse and what to do.
A progressive and incurable disease, COPD, which includes both emphysema and chronic bronchitis, requires close monitoring of symptoms if people are to avoid ongoing visits to the Emergency Department and stays in the hospital. “I’m finding that when people have a better understanding of what COPD is and how their medications work, they are better able to manage their symptoms,” says Spearing.
The majority, around 60 per cent, of KHSC patients with COPD are severely burdened by symptoms. Many of them are too breathless to leave the house or become breathless when getting dressed or undressed. Others have to stop for breath after walking a few minutes on level ground.
Since Spearing began her navigator role last fall, she has provided education to approximately 96 per cent of patients admitted with a primary diagnosis of COPD. As a Certified Respiratory Educator, she takes the time to make sure people understand when to take their medications and are using their inhalers properly. If they currently smoke, Spearing provides education and support while in hospital and can connect them to community resources that can assist in their ongoing attempt to quit.
As well, close to 90 per cent of patients receive a COPD Action Plan to take home, which lays out in colour what someone’s usual symptoms, activities and treatment are (green zone), what their symptoms and actions are when they are feeling worse (yellow zone), and what actions they should take when their symptoms are much worse (red zone). These plans are also shared with people’s primary care providers.
“The action plan is really effective for most people because it is simple, and clearly and visually explains what to do and when, so people have an easier time managing their symptoms at home,” says Spearing. For those who struggle with managing medications or understanding instructions, the action plan and other education can be challenging. “That is where family and friends, and referrals to community supports can be particularly helpful,” added Spearing.
The most common referral Spearing makes upon discharge from the hospital is to the Rapid Response Nurses from Home and Community Care, who visit patients in their homes to ensure they have what they need to successfully manage in their communities.
While many patients are already connected to the Respirology Clinics at KHSC’s Hotel Dieu Hospital (HDH) site, Spearing will refer people who are not and who could benefit from these services. Referrals are also made to the COPD Nurse Practitioner at the HDH site for people who do not have a primary care provider, and to Providence Care Hospital for people who would benefit from specific rehabilitation services.
“Kim’s role is one of the recommendations made by the regional COPD Steering Committee for southeastern Ontario,” says Delanya Podgers, Asthma and COPD Nurse Practitioner at KHSC. “It builds on the completion of the other recommendations to standardize documentation with which Kim and others work, including order sets, the discharge or care gaps checklist and the COPD Action Plan.”
Improving patient outcomes, as well as patient and provider satisfaction, and making the best use of resources will ultimately result in fewer COPD-related ED visits, hospital admissions and 90-day re-admissions, which were 1259, 585 and 155 respectively in the fiscal year 2017-18.
Gallery


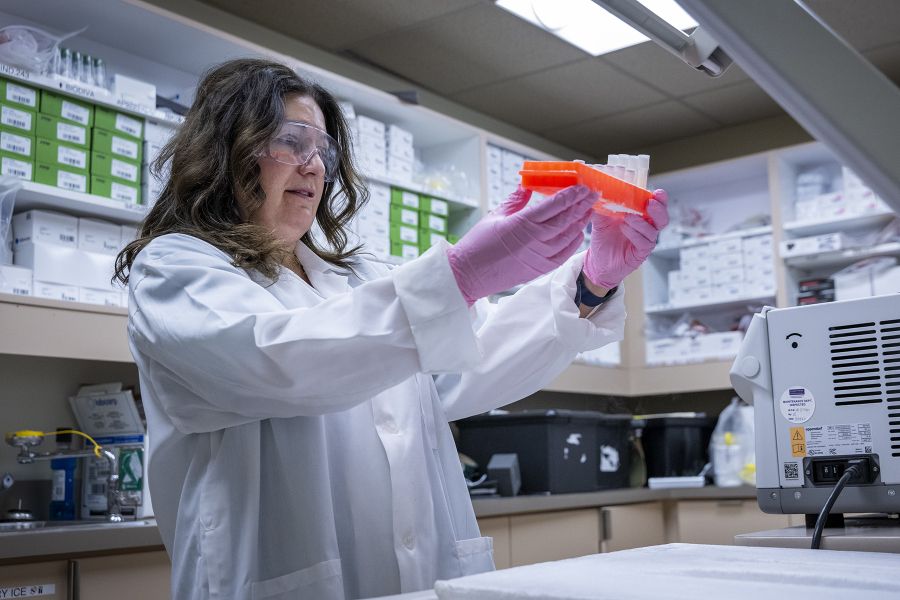
KHSC's COPD Nurse Navigator Kim Spearing reviewing medications with a patient in the Admission Transfer Unit at the Kingston General Hospital site.