Effective immediately masking is required for everyone when present on all inpatient units, in the Emergency Department (ED), the Urgent Care Centre (UCC), and the Children’s Outpatient Centre (COPC).

In a hospital that specializes in complex care such as cancer, stroke, cardiac and trauma, a pressure ulcer (also known as a bed sore) may seem like a minor medical condition. But for our patients, they can be quite painful, can lead to infection, and may result in a longer stay than necessary. It’s why KGH has made reducing them one of our top goals in this year’s Annual Corporate Plan.
A pressure ulcer is an injury that is caused by unrelieved pressure on the skin. They often develop on a patient’s heels, hips or buttocks and are more common in people with limited mobility, such as those confined to a bed or wheelchair for long periods of time.
“Right now we are focusing our efforts on three specific units, the Kidd 2 Intensive Care Unit, Kidd 6 and Connell 10,” says Jennifer Kasaboski, Pressure Ulcer Prevention Nurse. “We are now tracking the pressure ulcer prevalence numbers in these areas each month with an aim of reducing them by at least 25 per cent."
Then in February, this tracking will be expanded across KGH for one month, to give the prevention team a hospital-wide baseline to work with.
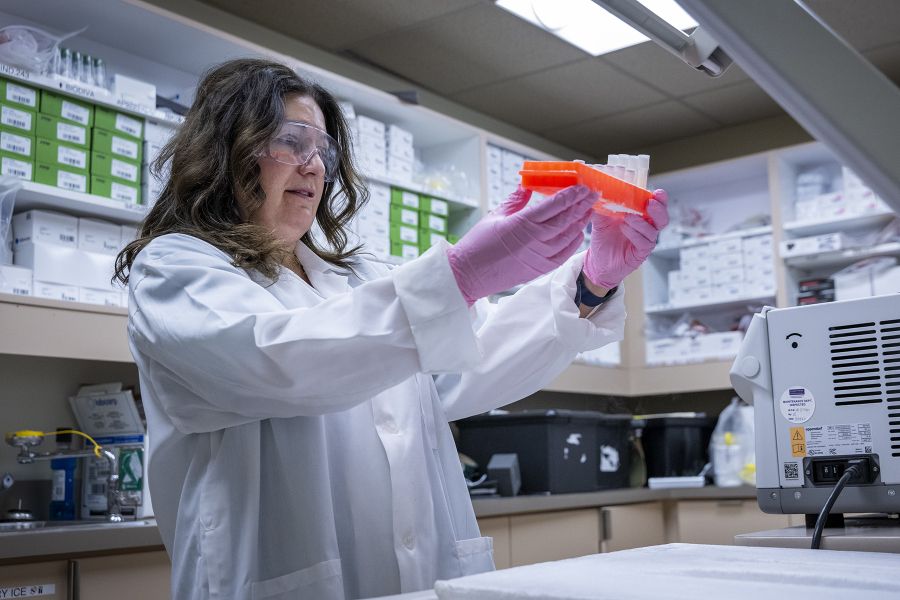
Recently, more than 50 nurses across the hospital received wound care training to become skin and wound care nurse champions. They are now acting as mentors in their units and providing education to their peers about how to prevent pressure ulcers from developing. This includes frequently turning patients to relieve skin pressure and helping them to return to their previous level of mobility as soon as possible.
A series of online training modules are also being rolled out to nurses and patient care assistants (PCA) to ensure they have up to date education on all pressure ulcer prevention best practices.
“With our increased attention and this new education, we are already seeing some improvements,” says Kasaboski. “Last quarter, we nearly reached our goal of a 25 per cent reduction and we estimate we were able to save roughly 27 patients from developing a pressure ulcer.”
Kasaboski says there is another simple thing we can do to ensure we are working with good data. “When patients are admitted to the hospital, it is important for our nurses to check for pressure ulcers during their initial patient assessment so we document them properly and also begin treatment."
Another important initiative that is helping protect our patients from pressure ulcers is our purchase of raft of new patient care beds. So far, we have bought 334 of the new Hill-Rom Advanta2 beds and each comes with a special mattress that’s designed to help prevent skin breakdown.
Last year, with funding assistance from the University Hospitals Kingston Foundation (UHKF), KGH also purchased more than 30 special mattresses for patients who are specifically at high risk for skin breakdown or have an existing pressure ulcer. The mattress is filled with air, from a compressor, which helps to reduce pressure on the patient’s skin.
“With all these measures in place, and thanks to the diligent work by our staff, we are seeing a lot of progress already,” says Leanne Wakelin, Interim Director of Professional Practice Nursing. “However, we still have some work to do to make sure we are protecting our patients as best as we can.”
Gallery


RN Julia John is one of KGH’s new skin and wound care nurse champions. Here she shares pressure ulcer prevention strategies with Nursing Student Scott Conway in the Kidd 2 ICU.