Effective immediately masking is required for everyone when present on all inpatient units, in the Emergency Department (ED), the Urgent Care Centre (UCC), and the Children’s Outpatient Centre (COPC).

National Nursing Week is a great chance to celebrate the hundreds of nurses who work at KGH. It's also an opportunity to shine the spotlight on a smaller group of nurses in our hospital, nurse practitioners (NP).
At the moment there are eight of them working in a range of services from acute and chronic pain, to cardiac surgery, to our outpatient Asthma clinic. And thanks to recent changes in provincial legislation, they are playing a bigger role here now than ever.
Along with diagnosing and treating common illnesses and injuries, NPs can now discharge patients from hospitals. Starting this summer they will also be able to admit them as well.
"A lot changed for us last fall," says Valerie Wilson, NP specializing in acute pain. "The new legislations allow us to write more medication orders and order more diagnostic and laboratory tests without medical directives that have to be signed by physicians."
Rosemary Wilson is KGH's longest serving NP. She works in acute and chronic pain and says the increased scope of practice for NPs is already contributing to more effective patient care.
"It levels the playing field and really enhances collaboration with our physician colleagues because they see we are accountable for our decisions," says Wilson. "It also saves time and makes us all more efficient."
According to the Nurse Practitioners Association of Canada, studies have shown that NPs can help reduce wait times and improve patient outcomes and satisfaction while also reducing health care costs.
Director of Professional Practice for Nursing Carol Kolga says that's not news to people who have worked with our NPs.
"They are a rich resource to all," she says. "Nurse practitioners offer timely access to care to our patients in a collaborative and highly skilled capacity."
NPs say their approach to medicine helps them support patients in a unique way.
"We look at patients from a very holistic point of view, encompassing medicine, nursing, rehabilitation and pharmacy as well as social aspects," says Valerie Wilson.
NPs also are able to spend a bit more time with each patient which can make a big difference.
"We are able to encourage patients and families to discuss issues they may not have had a chance to ask about yet," says Nicole Chenier-Hogan, NP in neurosurgery. "Our listening skills are well developed and we sometimes learn about key things that may be impacting their health."
Chenier-Hogan says NPs are also able to follow up with patients and their families once they are home. She hands out her card to all patients and encourages them to get in touch quickly if they have any questions.
"I get a lot of calls from patients wondering if a symptom they are experiencing is OK or if they need to be seen," says Chenier-Hogan. "Often this kind of consultation can end up saving them a trip back to our emergency department."
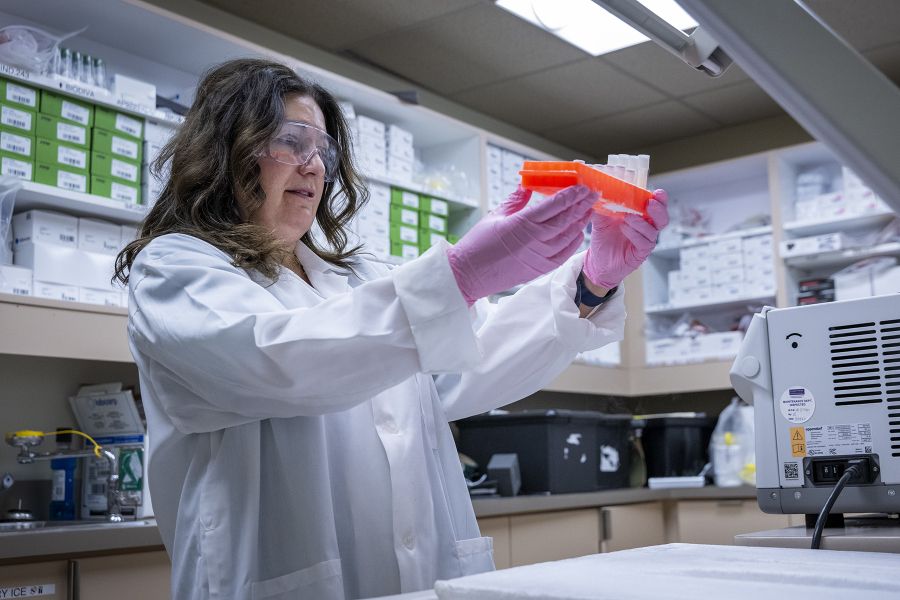
All of the NPs at KGH are also involved in clinical research.
Their projects are patient-oriented and are generated from their own practices. As an example, Valerie and Rosemary Wilson recently received some funding to work on a project looking at symptom management after total joint arthroplasty.
"We study things we can use the results from to change our practice and better care for our patients," says Valerie Wilson.
"We are a health oriented type of discipline. Everything we look at has the restoration of the patientss overall health in mind," adds Rosemary Wilson.
To learn more about NPs, visit the website of the Nurse Practitioners Association of Ontario's at http://www.npao.org