Nearly every person has been affected by cancer in some way, at some point in their lives. Whether it’s directly as a patient, as a care partner, or as a caring friend. Though it affects many, how it impacts each individual often differs.
A cancer diagnosis can significantly alter one’s emotional wellbeing, lifestyle and quality of life and, while there’s so much variability, a cancer diagnosis can create uncertainty and cause feelings of powerlessness. A diagnosis also often raises difficult questions and potential distress.
How do I tell my family?
What are my options and how will my body respond to treatment?
Can I afford to take time off work?
At KHSC, the Psychosocial Oncology Team is setting the standard for comprehensive cancer care by ensuring people have the resources and information they need to live well with cancer.
We look at the whole picture, not just the disease site. When you’re diagnosed, you bring your entire world with you. Everything from your relationships to financial obligations, lifestyle and daily habits will factor into your experience. - Jessica Bonney, program manager for the Southeast Regional Cancer Centre
Part of the Southeast Regional Cancer Program, the Psychosocial Oncology Team includes social workers, a patient educator, dietitians, speech language pathologists and a mental health nurse who work together to support patients.
The burden of cancer
“Our work is split between helping patients navigate practical issues and offering psychotherapy” says Social Worker Maggie McDougall. “People at times do not realize the burden that can come with cancer treatment. Taking time off work, for example, could mean a reduced income, and if you don’t have a support network it can become a major obstacle. Our goal is to clear the barriers so everyone has access to care.”
Article continues below.
Gallery



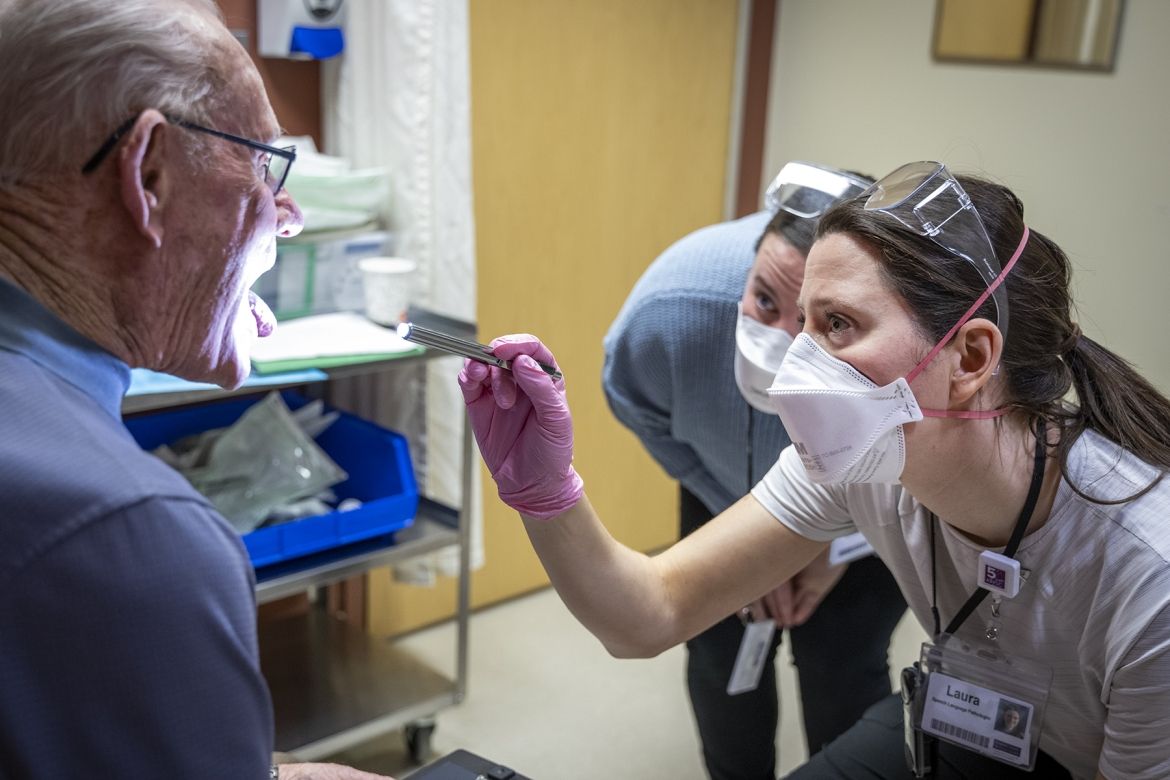
Speech pathologist Laura Mears meets with a patient
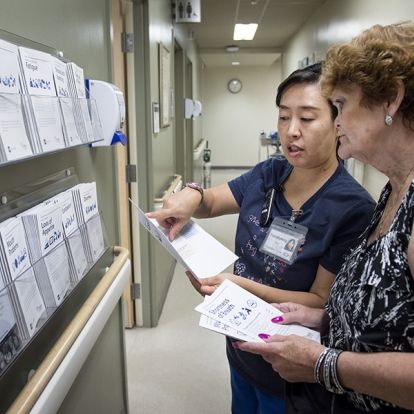
Once a patient is referred, the social workers use their expertise, to help patients and their care partners navigate the often-complicated processes that come with cancer care. This could mean ensuring that they are aware of the resources that are available to them to address practical needs, such as lost income and transportation.
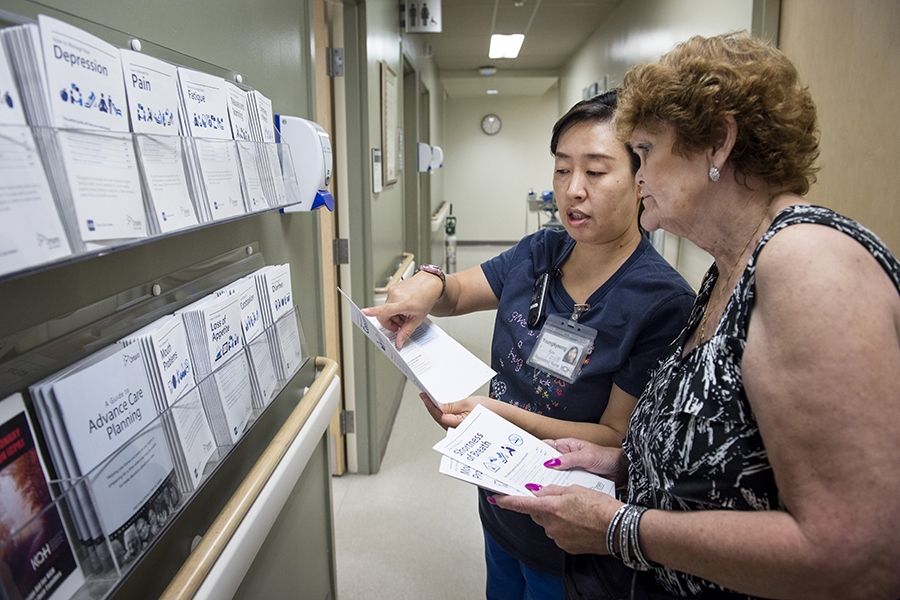
The team’s patient and family educator, Sarah Vanderhelm, works with the social workers to fill the knowledge gap. She maintains an extensive catalogue of resources and connects patients to the right information at the right time. This includes running weekly education classes to make sure patients feel supported.
Empowering patients
More specialized roles are also needed to ensure a patient has comprehensive care.
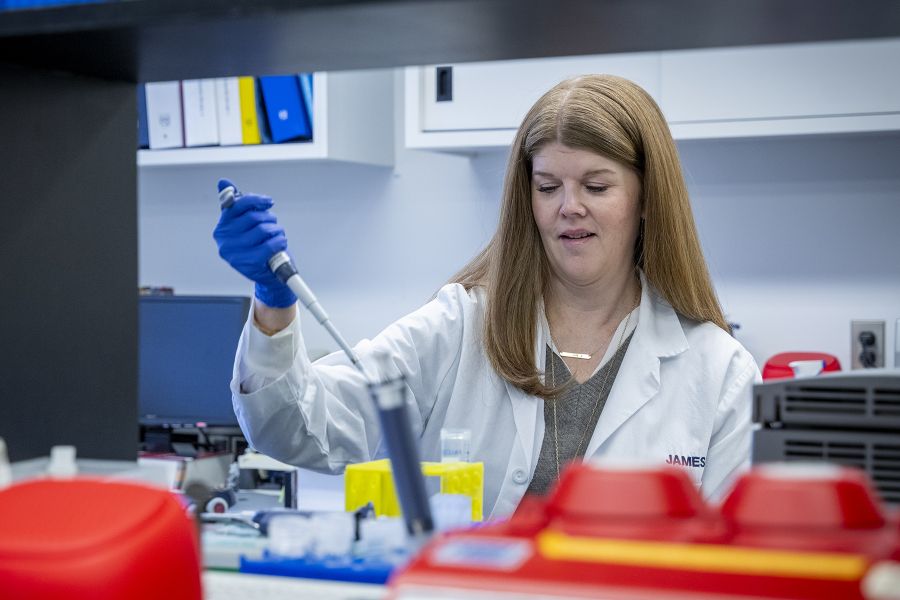
The team’s four dietitians help patients to meet their nutrition needs before, during and after treatment. Eating well can be challenging depending on the type of cancer and the treatments received. Maintaining good nutrition throughout a patient's cancer journey can help with weight maintenance, improve energy, strength and overall well-being, decrease risk of infection and assist the body with healing and recovery from cancer treatments.
The dietitians work with the patient and, often times, their support network to develop a plan to help them meet their nutrition goals. When developing plans, the dietitians take a comprehensive approach, accounting for a patient’s food preferences, cooking abilities, symptoms, financial situation and access to food.
“Nutrition is an important part of cancer treatment; as dietitians we help to educate and support patients with managing symptoms and meeting their nutrition goals throughout their cancer journey" says Hannah Kinstler, Registered Dietitian.
Within the team, two speech language pathologists (SLPs) focus on patients with head and neck cancers.
These cancers, and the interventions used to treat them (which could include, but are not limited to surgery or radiation), can cause swallowing impairments and difficulties speaking by affecting certain physiologic functions. This can increase the risk of aspiration (when food or liquids enters the lungs) and choking. SLPs work to help manage these risks, but it also comes back to agency:
It’s not just about swallow rehabilitation and improving communication, it’s about supporting, educating and empowering patients. Head and neck cancer can significantly impact a patient’s ability to eat and drink and to communicate. We help them to regain some of these functions, and as a result, they get a bit of agency back. It’s about helping them move forward after diagnosis and treatment. - Laura Mears, Speech Language Pathologist
Meeting patients where they are
A cancer diagnosis can mean difficult conversations for patients and their loved ones. It could mean a temporary disruption or a tragic reduction in life expectancy. The Psychosocial Oncology Team helps patients have these conversations by providing counselling.
“Sometimes it’s about how they’re going to tell their loved ones. Other times, it’s about helping them advocate for the end of life care they want,” says Social Worker Maggie McDougall. “This helps patients feel validated and supported through one of the most challenging times in their lives”.
The social workers work with patients to navigate feelings of anxiety, depression and grief, but when symptoms escalate, patients can be referred to Heather Campbell, the team’s dedicated mental health nurse who works alongside psychiatrist, Dr. Claudio Soares, in the Cancer Centre Mental Health Clinic. The Clinic was introduced by the program in response to a need for specialized mental health support for people living with cancer and provides another example of how the psychosocial oncology team is filling gaps in care.
“The goal for us is to stabilize a patient’s mental health so they can focus on treatment and day-to-day life,” says Campbell. “These things can have a negative impact on care outcomes and quality of life for the patient. Sometimes the goal is just to get the patient past anxiety and in the door to start treatment.”
Patients are provided with resources on practical techniques and strategies, but Campbell can also work with patients to develop a medication regimen. The goal is to ease the burden for patients and help them focus on what matters.
Everyone’s journey is different. For patients facing a terminal diagnosis, the psychosocial oncology team can help with the process.
“Counselling supports are available for caregivers too and patients are often just relieved to know that we’re able to support the ones closest to them,” says McDougall. “It can provide some peace of mind.”
Thanks to advances in treatment, more and more cancers are becoming highly manageable and even curable. For those on the other side of treatment, the team also helps with the transition to survivorship.
“Fear of cancer recurrence is one of the most common things we see,” says Campbell. “I’ve spoken with patients who still respond strongly whenever they drive by the hospital, even years later. We help patients put their cancer treatment behind them so they can focus on what’s ahead.”
The conversations are hard, but the psychosocial oncology team can help by filling gaps. It’s about taking a multifaceted approach to meet patients where they are.
“Cancer care treats a specific cancer at a specific site, but we treat the entire individual,” says Bonney. “To be truly successful, treatment has to involve more than physical care and interventions. We need to treat the whole person, including their emotional, functional and social health.”