Innovative cancer research treatments and practices by clinician-scientists and researchers at Kingston Health Sciences Centre, the Cancer Centre of Southeastern Ontario and Queen’s University have been recognized with funding from the University Hospitals Kingston Foundation (UHKF) and the Queen’s Cancer Research Institute (QCRI).
The awards will help investigators advance new knowledge and clinical practice in areas including colorectal cancer, melanoma, lung and bladder cancer, and radiation treatment for cancer patients.
“These grants highlight the breadth and novelty of patient-oriented cancer research being done locally by our clinician-scientists and researchers,” says Roger Deeley, Vice President, Health Sciences Research at KHSC and President & CEO, KGH Research Institute. “Internal grants play an important role in enhancing current research and stimulating funding from other sources.”
UHKF Interdisciplinary Cancer Research Grants target cross-disciplinary research by teams of two or more individuals from different disciplines or departments at Queen’s University, at least one of which must be a primary appointee from the Department of Oncology. This year’s ICRG recipients are:
- Dr. Nazik Hammad (Medical Oncology) with co-investigator Dr. Harriet Feilotter (Pathology and Molecular Medicine) - $40,000 to support research into the effects of metformin on colorectal cancer, with an aim of designing better treatment options for colorectal cancer patients.
- Dr. Chandra P. Joshi (Medical Physics) with co-investigators Drs. Timothy Hanna (Radiation Oncology) and Gabor Fichtinger (School of Computing) - $40,000 to support research and development of an innovative clinical orthovoltage radiation treatment planning system. This development will lead to improved treatment planning for non-melanoma skin cancer (NMSC) patients; and also provide a tool to compare outcomes in NMSC patients treated with orthovoltage radiation therapy.
- Dr. Douglas McKay (Surgery) and Dr. Timothy Hanna (Radiation Oncology) - $40,000 to support a population-based study of the quality of melanoma surgery and pathology reporting in Ontario, providing an understanding of the surgical management of melanoma in Ontario that up to now has been unavailable. This may influence provincial policies on organization of melanoma care and highlight potential opportunities for improvements that would benefit patients. Surgical quality improvement could lead to reductions in the treatment morbidity of recurrent melanoma, help maintain patient quality of life, and may potentially influence survival in some cases.
- Dr. Sunil Patel (Surgery) with co-investigator Dr. Chris Booth (Medical Oncology) - $38,900 to study how non-adherence to clinical practice guidelines affects long-term outcomes for rectal cancer patients and the barriers to care for those patients.
Queen’s Cancer Research Institute Translational Research Team Grants focus on high impact, clinically relevant questions pursued by teams of up to five members. This year’s recipients are:
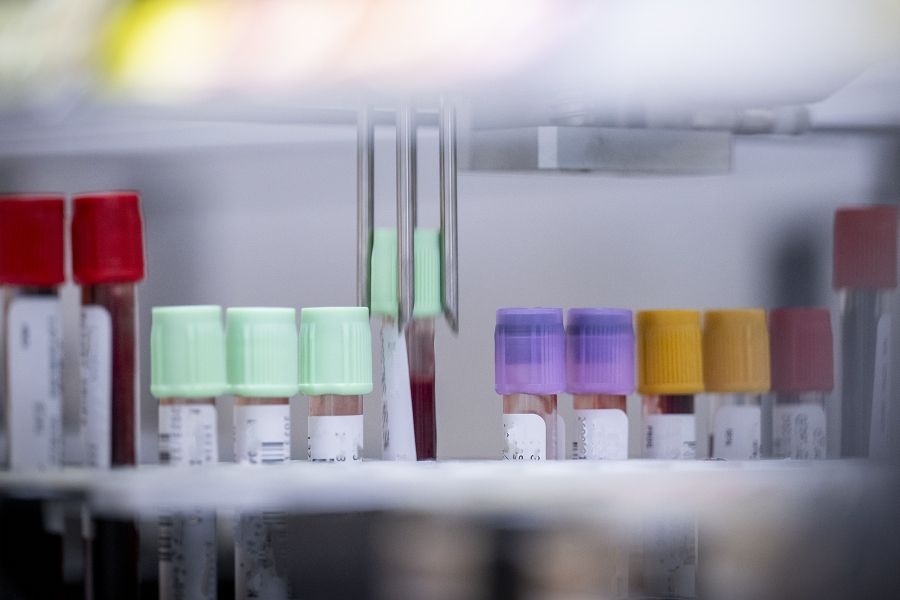
- The Genito-Urinary Research Unit, led by Dr. David Berman (Pathology and Molecular Medicine) - $40,000 to identify therapeutic vulnerabilities caused by common mutations in bladder cancer, and to develop a provincial bladder cancer tissue cohort. This collective knowledge will enable better targeting of particular treatments such as radiation, chemotherapy, immunotherapy and surgery, to specific subgroups of patients with bladder cancer.
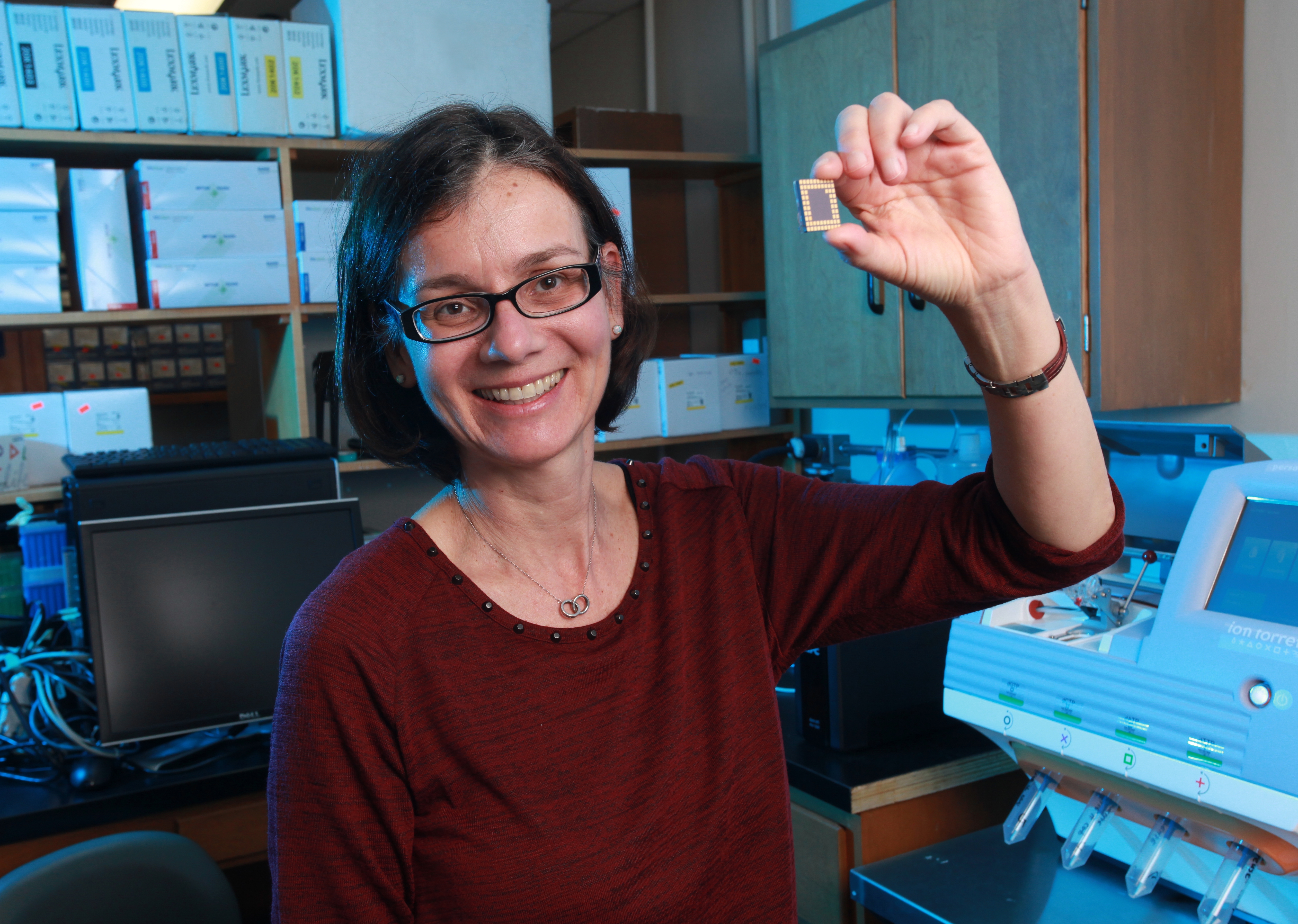
- The Lung Cancer Team, led by Dr. Harriet Feilotter, Principal Investigator (Pathology and Molecular Medicine) - $40,000 to study lung cancer tissue samples of patients undergoing immunotherapy treatment. The aim is to identify biomarkers to predict treatment benefit, show speed of response, and predict treatment toxicity (side effects), leading to better outcomes for lung cancer patients.
Gallery
Harriet Feilotter is leading a team investigating immunotherapy treatments for lung cancer, and is collaborating with Nazik Hammad on examining better treatment options for colorectal cancer.