Every few years a new piece of technology is released that can dramatically change the way medical teams provide care to their patients. Now, Canadian surgeons and researchers have partnered with a team in the U.K. to develop a tool that will transform the way cancer is surgically removed in the future.
During surgery, medical teams balance the need to remove all of a tumour, while at the same time not removing too much healthy tissue. In the operating room this is often complicated by the fact that tumours do not have smooth edges.
"Often a patient will ask after surgery if we were able to remove all the cancer," says Dr. John Rudan, head of the Department of Surgery at Kingston Health Sciences Centre (KHSC) and Queen's University. "Sometimes it's hard to tell if all the cancer has been removed until the tissue is tested in a lab. This can mean that patients may have to undergo a second surgery if some of the tumour was missed. We hope our new tool will one day help solve this problem."
The tool, known as the NaviKnife, combines an “intelligent” surgical tool called the iKnife, developed at Imperial College in London, England, with real-time mapping capability developed at Queen’s. The iKnife, which heats and cauterizes tissue as it cuts, uses mass spectrometry to analyze the smoke that is produced from each cut and can 'smell' if the tissue was cancerous.
"It's an excellent piece of technology and by partnering together we will be able to improve the device even further," says Dr. Rudan. "Currently it can tell the surgeon they have cut too close to the tumour. We hope that by adding visual mapping to the tool it can help surgeons avoid the cancerous tissue all-together. This partnership could really result in a transformative technology for surgical teams."
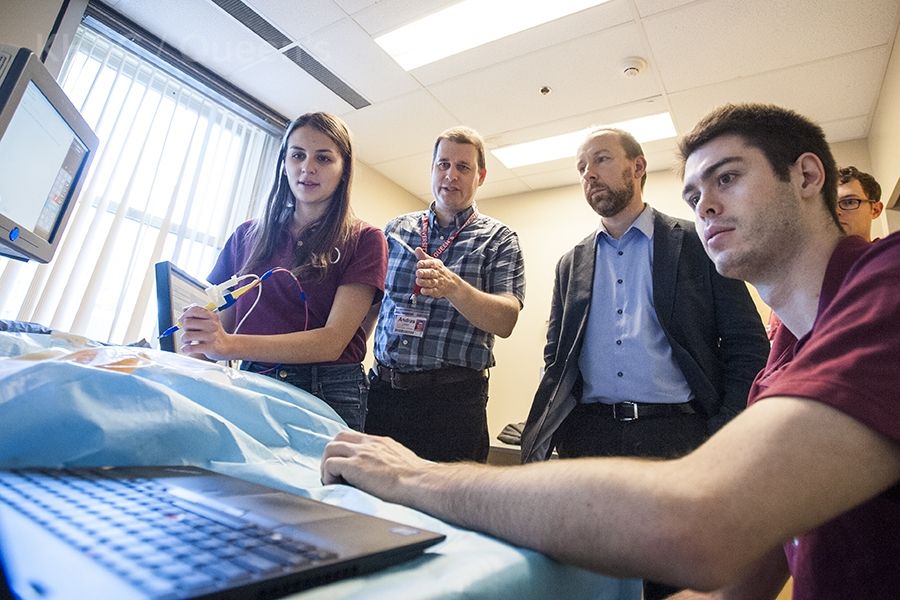
Kingston was chosen to partner in the development of the NaviKnife because researchers in Queen's University's Laboratory for Percutaneous Surgery (Perk Lab) have developed an international reputation for their work in surgical navigation technology. The Perk team has created a mapping technology that allows surgeons to visualize a tumour in 3D which can help them minimize their risk of disturbing the tumour as well as the loss of any healthy tissue that surrounds it.
"Queen’s research expertise will be used to develop spatial awareness in the iKnife," says Dr. Gabor Fichtinger, Professor and Cancer Care Ontario Research Chair, Queen's School of Computing. "This new technology will offer for the first time, real-time definition and pathological analysis of the tumour margins during surgery. It will allow surgeons to remove cancerous tissue with precision, decrease the incidence of positive margins, and thus avoid repeat surgeries and systemic therapies.”
Currently, the iKnife is an investigative research and surgical tool. Kingston will become the first city in North America to have access to the technology, joining a small number of centres in Europe. Intensive research will be done over the next several years at Queen’s with the iKnife being used in the operating rooms at Kingston Health Sciences Centre.
"This partnership is a great example of the global reputation Kingston is developing in medical research," says Rudan. "This partnership says that Queen's University and Kingston Health Sciences Centre are leaders in this area of research and patients around the world may one day benefit from our expertise."
Gallery
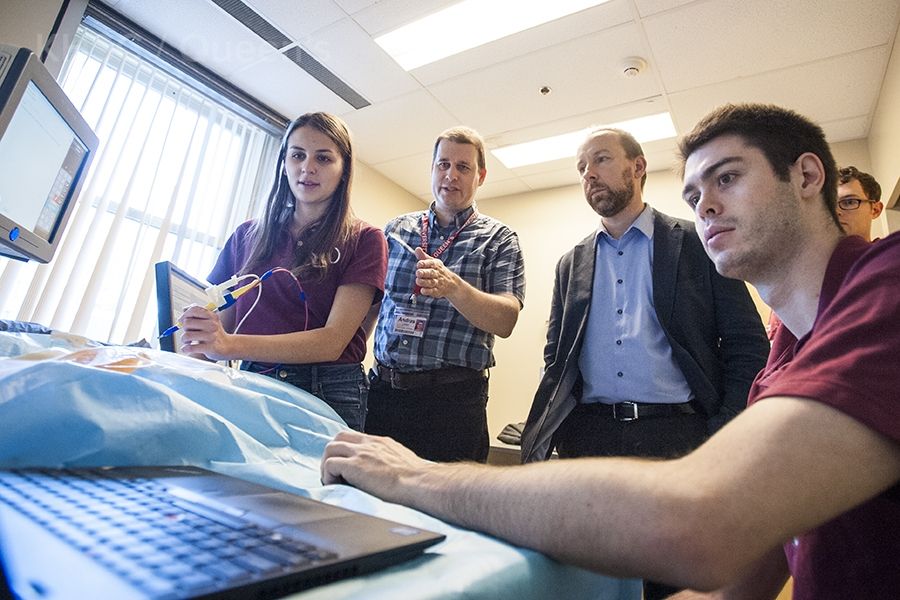
Dr. Zoltan Takats, inventor of the iKnife receives a demo of the visual mapping technology from the Perk Lab team