Effective immediately masking is required for everyone when present on all inpatient units, in the Emergency Department (ED), the Urgent Care Centre (UCC), and the Children’s Outpatient Centre (COPC).

A new study out of Kingston Health Sciences Centre (KHSC) is helping to shed some light on a serious but often misunderstood health condition. Delirium has been shown to have critical long-term impact on the most seriously ill patients, but still has no known cause.
For former KHSC patient Robert, the first sign that something wasn’t quite right was when he began noticing fruit flies in his home. However, he was the only member of his household to see them.
“He would see people that weren’t there and hear sounds that no one else could hear,” says his wife, Joanne. “That was when I started to get concerned that something serious was happening.”
It was in the Urgent Care Clinic at our Hotel Dieu Hospital site when Robert first heard the word delirium.
“I had no idea what they were talking about, or what delirium meant, or that it had anything to do with how I had been feeling, “says Robert. “Hearing the word delirium was a totally new term to me.”
Lack of public understanding or awareness of delirium is not a surprise to Dr. Gord Boyd, a KHSC critical care physician and assistant professor at Queen’s University. In fact, delirium is a topic that Dr. Boyd has been researching to better understand its nature and long-term consequences in order to help draw attention to this important health issue.
“When a patient becomes critically ill their body undergoes tremendous stress and the brain starts to function abnormally, which is known as delirium,” says Dr. Boyd. “Broadly, delirium is an acute change in level of consciousness that fluctuates throughout the day and can cause impaired attention, delusions and hallucinations and it exists across the spectrum of care, from emergency departments to hospital wards and long-term care facilities.”
Currently, there is no known cause or treatment for delirium; however that may soon change. Dr. Boyd and a team of colleagues recently completed a study to demonstrate that low oxygen levels in the brain are a risk factor for developing delirium in an Intensive Care Unit (ICU). This study was the first of its kind to be done and is now expanding to other health care centres for further validation.
“It’s important for us to understand the underlying cause of delirium so we can help improve the outcomes for our patients,” says Dr. Boyd. “We know that delirium is associated with every negative patient outcome and can have a long-term impact on a patient’s health and lifestyle including cognitive impairment, depression and short-term memory loss.”
Delirium can be so impactful that it has been shown that only 50 per cent of patients who were previously employed can return to their regular working status after experiencing delirium. Though there is no known cure, there are strategies in place that Dr. Boyd and his team use as part of an ICU Follow-Up Clinic to help patients transition back into their regular routine once discharged from the hospital.
As part of this clinic, patients return to the hospital at the three and 12-month mark after their discharge from the hospital to do memory recall tests and visit their ICU room, as well meet the people who took care of them to help anchor their memories.
“Having the opportunity to return to the hospital and meet and thank the staff who took care of me was incredible, I cannot say enough positive things about the ICU staff and nurses,” says Robert. “The care and therapies they used during my time in the hospital, and after, have been a big help in helping me to recover.”
March 14 is World Delirium Day and to learn more you are encouraged to follow the conversation on twitter using the hashtag #WDAD2018
Gallery


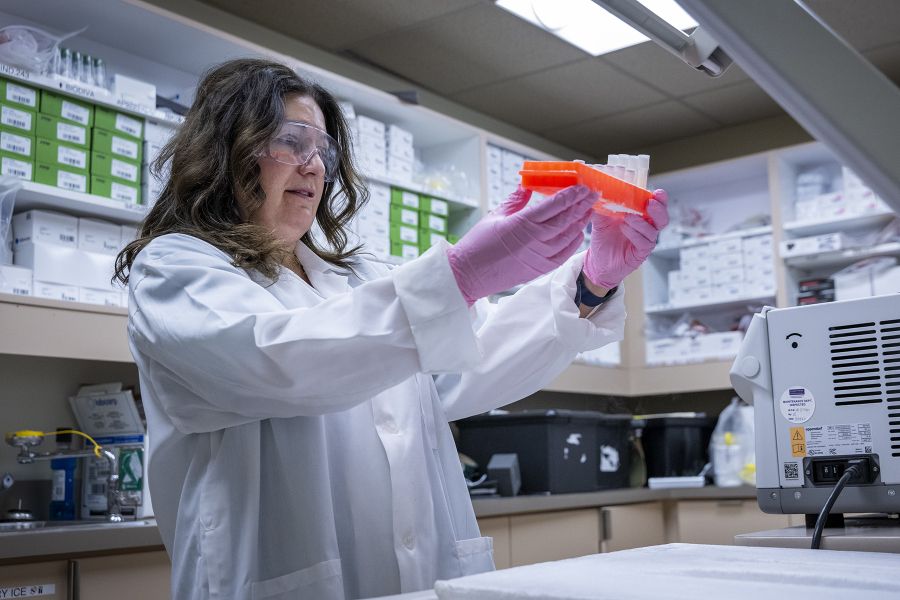
Dr. Gord Boyd meets with patients at the three and 12-month mark after their discharge from the hospital as part of their delirium care