Effective immediately masking is required for everyone when present on all inpatient units, in the Emergency Department (ED), the Urgent Care Centre (UCC), and the Children’s Outpatient Centre (COPC).
Over 50 per cent of people in developed countries will experience at least one episode of low back pain during their lifetime. Back pain is a common reason patients see their family practitioner and is responsible for more than half of opioid prescriptions.
“Back pain can affect your ability to work, play, and live a happy life,” said Savvas Frantzeskos, Advanced Practice Physiotherapist and Practice Lead for the Rapid Access Clinics for Low Back Pain (RAC-LBP) at Kingston Health Sciences Centre’s (KHSC) Hotel Dieu Hospital (HDH) site. “Knowing how to manage it can make all the difference.”
The RAC-LBP (formerly known as ISAEC) is an innovative, shared-care model through which patients receive rapid low back pain assessment (less than four weeks on average), education and evidence-based self-management plans. It is designed to improve outcomes for patients with persistent lower back pain, reduce unnecessary diagnostic imaging and specialist referrals, while facilitating access to these services when appropriate.
“Low back pain has similarities to the common cold. Most people get it and it’s not completely curable but if it’s managed properly, it is less likely to become a serious problem that negatively impacts our quality of life in a big way,” says Frantzeskos.
The role of the clinic is to provide direction on the best ways to manage different types of low back related pain. Most back pain can be effectively managed (without imaging) through appropriate exercise, and activity modification with or without a course of medication and treatment (e.g. physiotherapy, chiropractic, massage, etc).
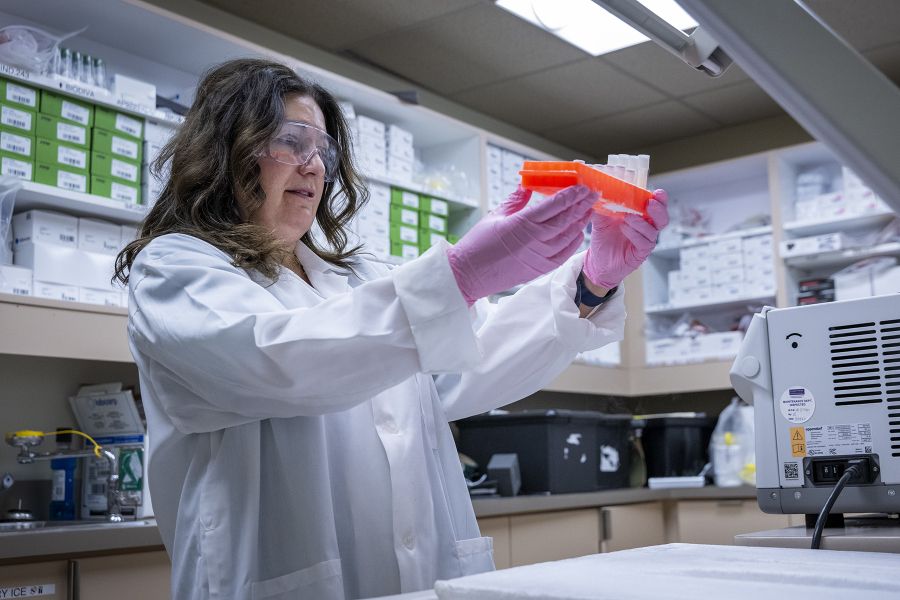
Among the specially trained team working with the RAC-LBP are Advanced Practice Providers (APP’s) who are community based physiotherapists and chiropractors who help guide the patient’s care.
“Often primary care providers do not have sufficient time to address all the factors contributing to someone’s persistent back pain. We have the gift of time.” says APP Randy Booth PT PhD. “APP’s spend up to an hour with a patient at their initial visit to assess and provide a treatment plan as well as a summary of recommendations to the primary care provider. Education on self-management and appropriate treatments can help reduce opioid initiation, ER visits, and the prevalence of chronic low back pain. “
In some cases, imaging, injections, and surgical opinion play a role. The program can coordinate these services to assist primary care providers.
"The clinicians working for RAC-LBP have the expertise to identify the most appropriate care for those suffering from lumbar related pain. The program also improves access and patient selection for surgical consults in cases that may benefit from surgical intervention,” says Dr. Daniel Borschneck, Orthopaedic Surgeon.
The RAC-LBP provides a collaborative approach to the management of a common and often disabling problem. Both patient and referring practitioner satisfaction rates are very high with 98 per cent of surveyed patients saying they were satisfied with their low back pain visit.
"The RAC LBP program is a great resource for both practitioners and their patients in terms of managing low back pain,” said Dr. Andy Ross, a local family physician. “The group provides a timely and knowledgeable service to the community. They have worked hard to fill a gap in care, leveraging their clinical skills and connections with hospital services to facilitate appropriate treatment plans for their patients."
A former patient, Jim Keech, shared his experience. “I have always had a very active lifestyle and was shocked when overnight severe back pain and sciatica made most normal activities, including putting on socks and shoes close to impossible. I was referred to the RAC-LBP program by my family physician after finding painkillers were providing very minimal relief. The APP was able to diagnose my problem without an MRI and made recommendations that helped me recover. I was able to resume my triathlon training and return to my normal work/life activities. About a year later we did a virtual follow up that helped significantly in reinforcing what I need to continue to practice.”
The service is free and available to eligible patients over the age of 18 as long as their primary care provider is enrolled with RAC-LBP.
In the South East region, clinics are located in Kingston, Belleville, Smiths Falls, and Bancroft. When appropriate virtual and telephone assessments can be arranged.
For more information, please visit: www.lowbackrac.ca or contact Savvas Frantzeskos at 613-544-3400 x 2328.
If you are a PCP who has yet to enroll with the program, please visit: https://www.lowbackrac.ca/refer-to-rac-lbp.html