Kingston General Hospital (KGH) has been designated by the Ministry of Health and Long-Term Care (MoHLTC) as one of ten hospitals across Ontario to serve as a referral hospital to treat confirmed Ebola cases. This means that patients with a confirmed Ebola diagnosis will be transferred to KGH after the necessary screening and initial assessment by their original receiving hospital is complete.
We have been chosen as a designated referral hospital because we have the full range of medical expertise to care for these patients in addition to the sophisticated infection control systems in place at all Ontario hospitals to limit the spread of infection. Our primary goal at all times is to protect all our healthcare workers and provide the best possible care for patients suffering from Ebola. We will continue to work closely with the three Public Health Units and all our partner hospitals in the South East LHIN to assist them in identifying and managing any suspected Ebola cases. All confirmed Ebola cases in our region will be transported to KGH in specially equipped air or ground ambulances that have been equipped with the appropriate personal protection equipment to keep Emergency Medical Services providers safe.
KGH has been busy preparing for potential Ebola cases since August and is in the final stages to be fully equipped to handle any potential patients. Late on Friday, October 17, the Minister of Health and Long-Term released a document of directives for hospitals involved in the care of Ebola patients. We have reviewed these directives and can confirm that with updates our hospital protocols meet all directives. Our first priority is to ensure that our staff are and feel safe when providing direct patient care and all patients suspected or confirmed of having Ebola receive the best possible care. A critical part of fulfilling this directive will be to ensure that front line care providers have all the necessary protective equipment and training so they feel comfortable and supported at all times.
1. What is the Ebola Virus?
The Ebola virus disease is a severe, often fatal illness. Ebola first appeared in 1976 in two simultaneous outbreaks, one in a village near the Ebola River in the Democratic Republic of Congo, and the other in a remote area of Sudan.
The origin of the virus is unknown, but fruit bats in Africa are considered the likely reservoir of the Ebola virus based on available evidence. In Africa, humans become infected when they handle or eat bush meat or partially eaten fruit dropped by the bats. Infected humans may then pass the virus from person-to-person.
2. How do people become infected with the virus?
Infection occurs from direct contact through broken skin or mucous membranes with the blood, or other bodily fluids or secretions (stool, urine, semen) of infected people. It is important to note that Ebola is NOT an airborne infection.
3. What are typical signs and symptoms of infection?
Sudden onset of fever, intense weakness, muscle pain, headache and sore throat are typical signs and symptoms. This is followed by vomiting, diarrhea, rash, impaired liver function, and in some cases, both internal and external bleeding.
The incubation period, or the time interval from infection to onset of symptoms, is from 2 to 21 days and anyone who becomes ill more than 21 days after exposure does not have the disease. Unlike the flu, unless symptoms are present, a person cannot transmit the infection. Exposure to a person before they develop symptoms does not pose a risk for transmission.
4. What is the chance of seeing a case of Ebola in our community?
The risk is very low and it is very unlikely that we will see a confirmed Ebola case in Kingston. At the moment, the disease is still centred in three countries in West Africa: Guinea, Liberia and Sierra Leone. The most likely scenario for a confirmed Ebola case is an individual who would have travelled to West Africa, had direct contact with an Ebola patient and be displaying symptoms. However, we do expect that we will see some suspected cases that turn out to be negative for Ebola.
5. What is KGH doing to prepare?
As part of our focus on patient safety, KGH is always working hard to eliminate the spread of hospital-acquired infections. To prepare for the potential arrival of Ebola cases, we have put in place some extra safety precautions including:
- Special screening procedures at all intake points to the hospital, including outpatient clinics. This screening process has been in place since August 5 and includes questions to determine if any patient has a fever and a recent travel history to West Africa.
- Training for staff in key areas such as the Emergency, Critical Care and Environmental Services departments, as well as for physicians on how to properly use enhanced personal protective equipment. This training is now being rolled out across the hospital.
- Isolation measures for any suspected Ebola patient include Enhanced Contact and Droplet Precautions. This includes a buddy system for donning and doffing personal protective equipment monitored by an Infection Prevention and Control staff member. Patients will be isolated in special rooms that allow areas for staff to don and doff personal protective equipment (PPE).
- Extra PPE for our staff has been procured; including enhanced protective equipment such as fluid resistant coveralls, goggles, face shields and fluid resistant boot covers. All PPE meet Ministry of Health standards set out in the new Ebola directives.
- We have mapped routes through the hospital, if a patient with a confirmed case needs to be transported (Emergency Department to ICU) to ensure they remain isolated from other patients, staff, visitors, etc.
- Special training is also taking place to ensure that our specimen collection and clinical laboratory teams are prepared should any blood specimens need to be tested. These specimens will be treated with special precautions, and laboratory staff will be advised prior to their arrival.
- An infectious disease specialist and an Infection Prevention and Control practitioner will be available for our staff 24/7 in case a suspected case arrives at KGH.
- KGH has been working closely with other hospitals, the South East Local Health Integration Network as well as the Ministry of Health and Long Term care to develop regional and provincial strategies for Ebola response.
6. Where can I find more information?
Ministry of Health and Long Term Care
Public Health Agency of Canada
Gallery


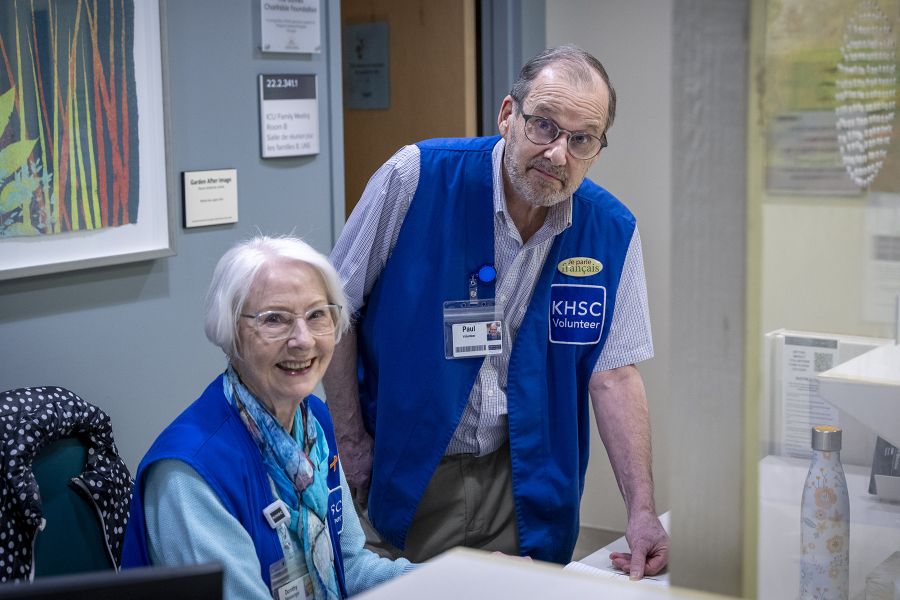
Staff at Kingston General Hospital work together in pairs and train on how to properly use enhanced personal protective equipment.