Effective immediately masking is required for everyone when present on all inpatient units, in the Emergency Department (ED), the Urgent Care Centre (UCC), and the Children’s Outpatient Centre (COPC).

A patient's journey through Kingston General Hospital can be as complex as the hospital itself, with stops at many different departments, floors and specialized units. We know patients and families want this journey to be as smooth and efficient as possible. We also know that staff and physicians want this to be better for patients. It's why we've made it a top priority to eliminate all preventable delays to, within, and from KGH.
To help us achieve this, we set bold targets and are monitoring closely how long patients are waiting for their surgery, or to be admitted to an inpatient bed, as well as how long they are staying in KGH once they are admitted. We've made a lot of progress in many areas but KGH recognizes there is still much work to be done - a situation brought into clearer focus by an increase in the situation we call "Code Gridlock." Our hospital calls a Code Gridlock, essentially, when there are significant delays in moving patients through the hospital to areas where they need to be. Once itís called, staff know extra measures are required to get the patient flow moving again, while also maintaining safe and quality care.
Over the past year, our Code Gridlock calls have been increasing in both frequency and duration. There are many factors contributing to this situation, including an increase in the number of patients visiting our Emergency department and a significant increase in the number of patients who then need to be admitted to one of our inpatient beds. At the same time, we are experiencing a more than doubling in the number of patients at KGH designated as being Alternate Level of Care (ALC). These patients are typically waiting for spots in long-term care facilities and no longer need to be in KGH for care.
All in all, it's a complex problem, but one that KGH is committed to solving.
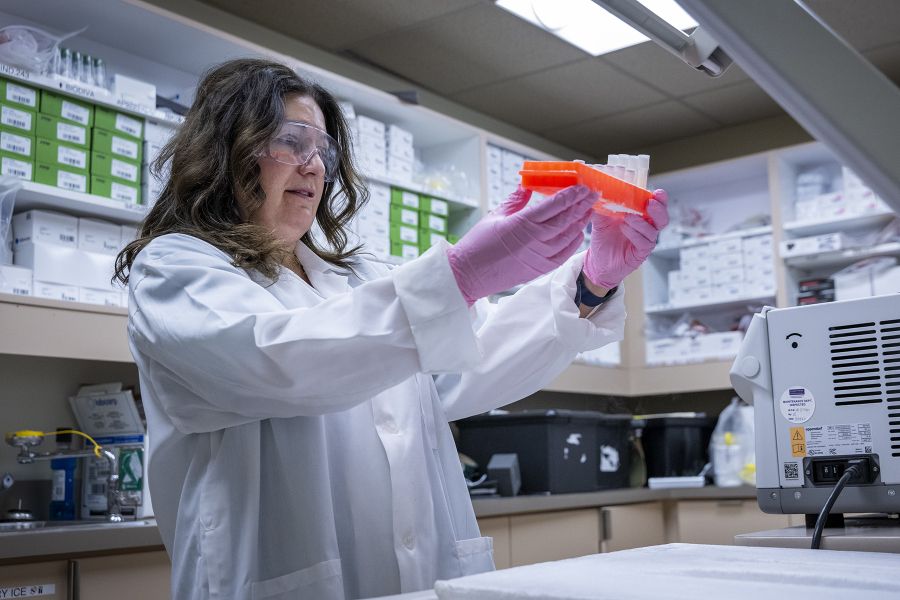
Here's how: over the next year, a big team of staff and physicians will be using the principles of continuous improvement to study the process of how patients move through our hospital, with a focus on where there are variations in process and on the delays. Then, rather than 'troubleshooting' solutions, will we start an ongoing process of identifying the root causes of these challenges, planning 'improvement cycles' and embedding sustainable changes to improve our performance.
And we won't be doing it alone. We have invited key regional health care partners to be part of this process, including Community Care Access Centre, Providence Care, family physicians, transportation providers and representatives from the province's Health Links initiative.
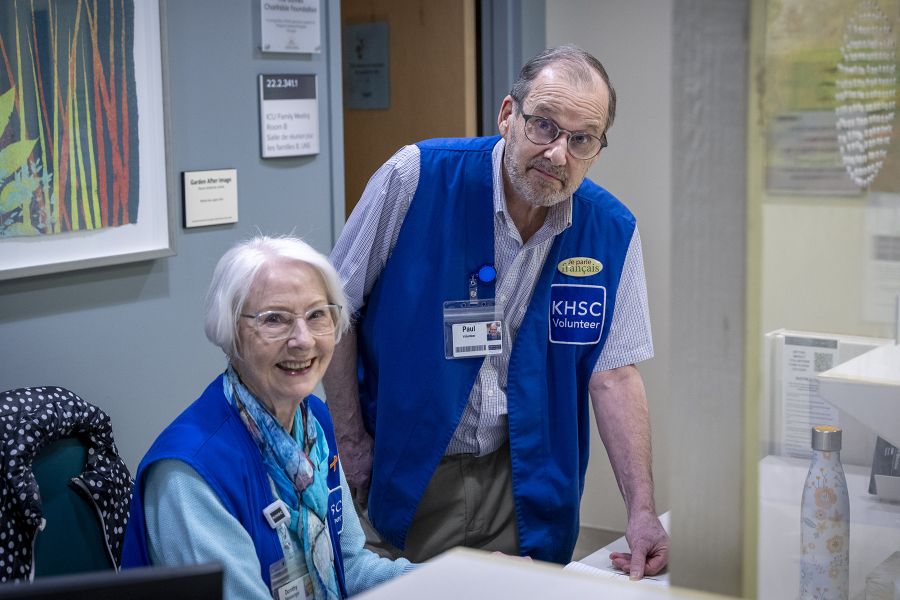
Altogether, a group of 75 people came together recently at KGH to begin this important work.
"Together we are developing a shared understanding of exactly what's contributing to these delays in the patient journey, and will use the insights of those working most directly with the processes to design innovative and timely solutions,' says Eleanor Rivoire, Vice-President of Clinical Administration, Professional Practice and Chief Nursing Executive.
"We have started by identifying four causes of delay and have started work right away to study and redesign those processes over the next 90 to 120 days. We will then move on to the next four and keep working until we see the number of Gridlocks reduced and see patient flow working well."
"We know that a tremendous amount of effort has brought us to this point and we are committed to making more progress and seeing this process through," says Rivoire. "Everything is on the table to achieve this goal and to transform the overall experience for our patients."
Gallery


Staff participate in a two-day continuous improvement session recently, aimed at identifying the root causes of gridlock.