It wasn’t so long ago that KGH was known for our struggles to prevent the spread of C. difficile infections (CDI) in our hospital. But a lot has changed over the last few years, and the latest numbers show KGH is performing very well on this important measure.
“Our infection rate has been trending steadily lower and we are very happy as it reflects improved patient safety,” says Dr. Gerald Evans, Medical Director of Infection Prevention and Control. “If you look at the Ontario-wide data and our peer hospitals, we are now on the very low end of CDI rates in hospitals, rather than way up on the high end.”
During the month of February, KGH reported two cases of C. difficile acquired by patients while in hospital and one case from a non-KGH source. This translates into a publicly reported rate of 0.17 cases per 1,000 patient days at KGH, compared to 0.24 for Hamilton Health Sciences, 0.75 for Sunnybrook Hospital and 0.88 for The Ottawa Hospital. It’s also been almost two years since KGH had its last publicly-declared outbreak of C. difficile, as the last one ended on May 1, 2012.
So what’s behind this dramatic improvement? Several initiatives are all contributing to our lower-than-ever CDI rates. One of the big ones is our Antibiotic Stewardship program. It’s been helping to control the inappropriate use of antibiotics, as antibiotics are known to trigger C. difficile infections in vulnerable patients.
Another factor is our use of a highly sensitive laboratory test that quickly lets staff know if a patient is infected with C. difficile so they can be isolated and treated.
Our Infection Prevention and Control team has also been monitoring all CDI incidences closely and working with patient care units to ensure early identification and prompt isolation. It also recently introduced a new C. difficile Infection Order Set for physicians to use. It’s a set of clinical guidelines that reflect best practices when it comes to managing patients with the infection.
Our decision in 2012 to stop screening and isolating patients for Vancomycin-Resistant Enterococci (VRE) may have also contributed, as it freed up resources for the fight to control C. difficile.
“Along with all these corporate initiatives, praise has to go out to people all over the hospital for the work they have been doing. It’s been a real team effort to make sure our environment is kept clean, that patients are isolated when they need to be, and that everyone is practicing proper hand hygiene at all times,” says Evans.
So what’s next? One goal this year will be to get our hand hygiene rates all the way up to 100 per cent for starters.
Another focus will be on improving our screening rates for another infection, Methicillin-resistant Staphylococcus aureus (MRSA). Anyone who has spent time in a hospital within the past year is supposed to be screened for the infection using a quick nose swab, but rates vary widely across the hospital, from about 100 per cent compliance down to 10 per cent in others.
“The bar on infection control is always moving so KGH will continue to look at our processes and seek new ways to eliminate all preventable harm to our patients as spelled out in our corporate strategy,” says Darlene Campbell, Manager of Infection Prevention and Control.
Gallery


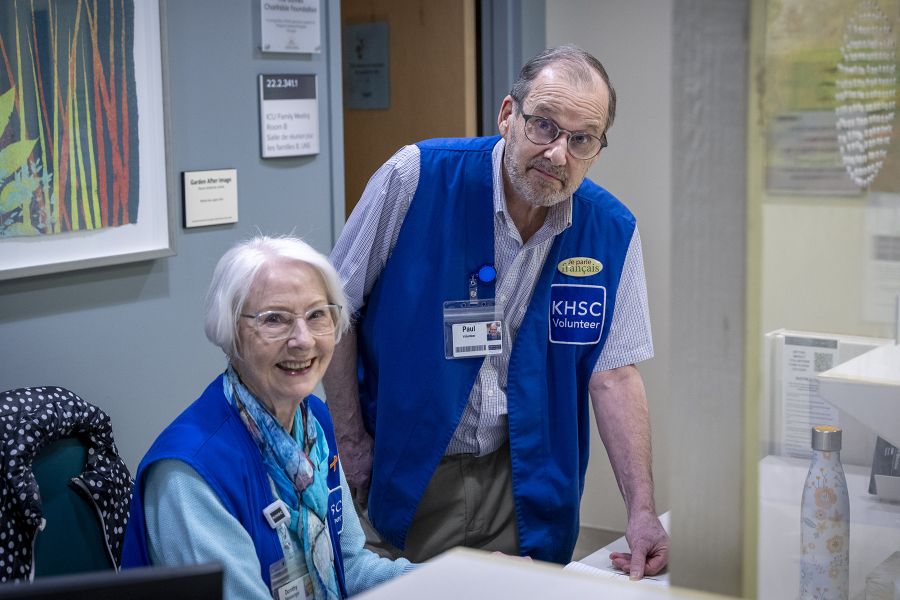
An auditor in our Emergency Department keeps an eye on staff hand hygiene practices. Hand hygiene is one of the keys to controlling the spread of infections such as C. difficile.