Effective immediately masking is required for everyone when present on all inpatient units, in the Emergency Department (ED), the Urgent Care Centre (UCC), and the Children’s Outpatient Centre (COPC).
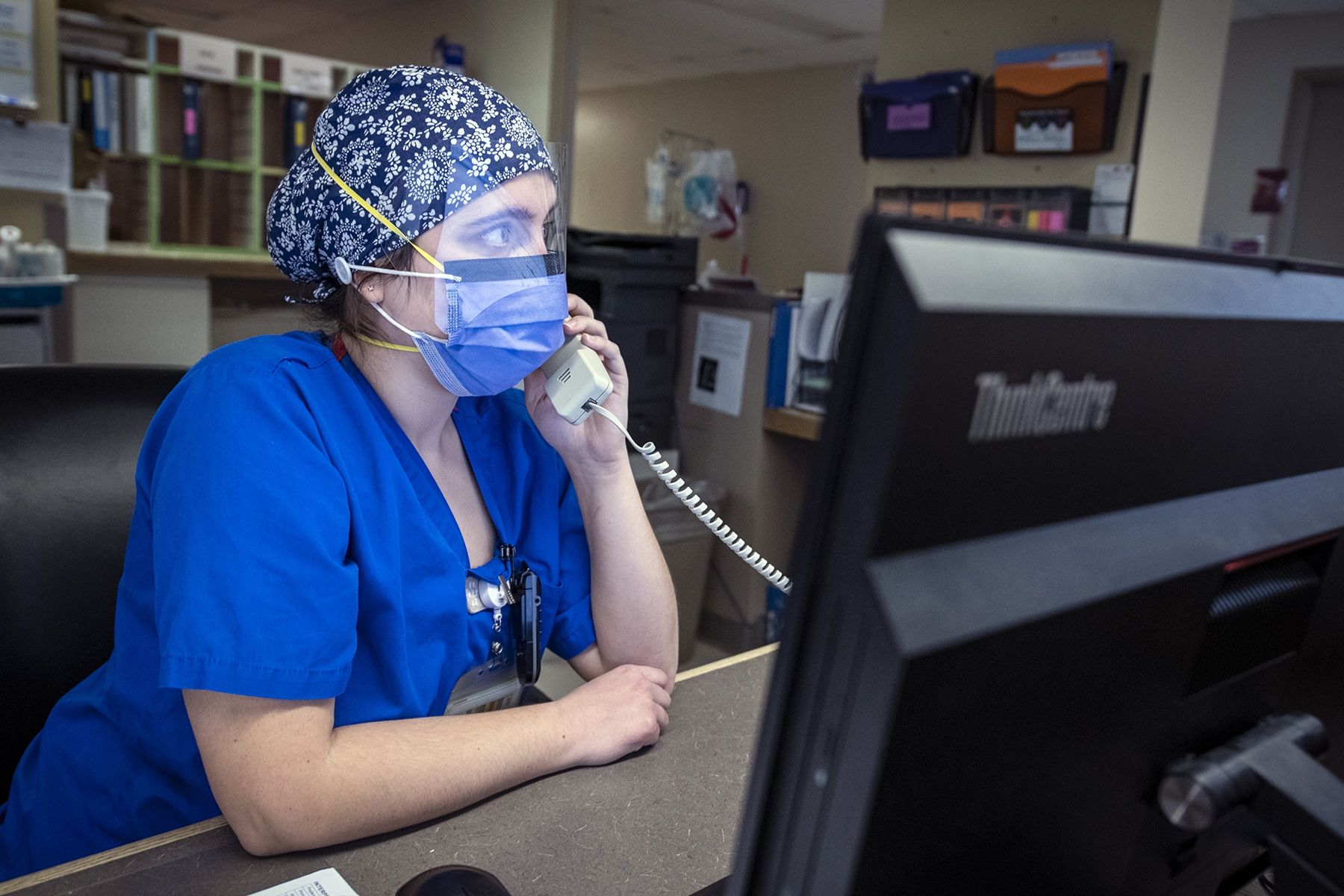
While most of the discussion during Ontario’s third wave of the COVID-19 pandemic has focused on bed space for critically ill patients, hospitals across the province are working hard to increase the number of staff to care for them.
“A hospital bed and equipment such as a ventilator are absolutely vital, but do little to save someone’s life without the specially trained teams required to deliver care,” says Dr. Mike Fitzpatrick, KHSC’s Chief of Staff. “The biggest issue currently is having the staff to care for these and other patients with urgent needs.”
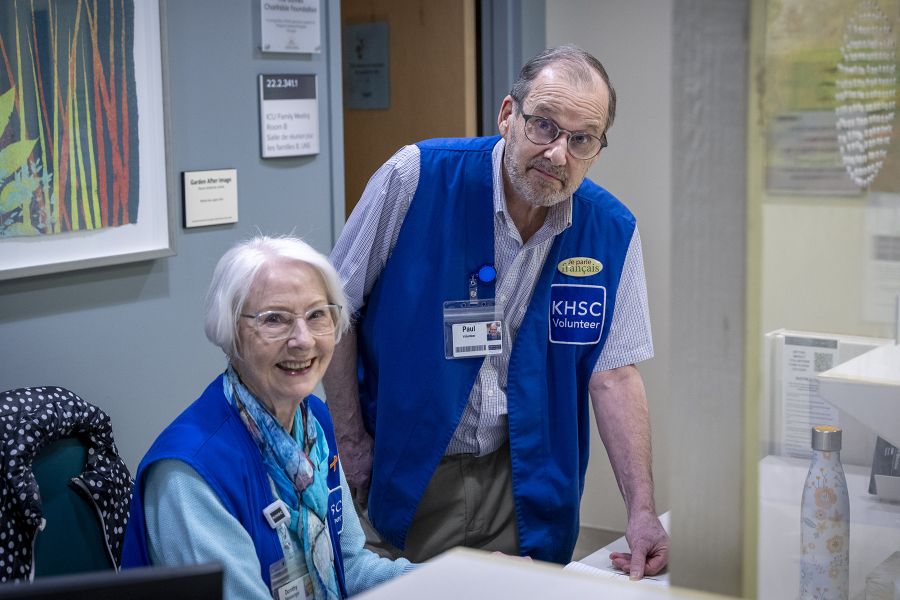
In response, Kingston Health Sciences Centre (KHSC) has been working since early April to identify nurses, allied health professionals and administrative staff across the organization who could support the surge of critically ill patients from other areas of the province. To date more than 200 staff members have been retrained and redeployed at KHSC.
Earlier this month, Ontario Health ordered hospitals to begin ‘ramping down’ non-urgent and elective care to allow the health care system to focus on the COVID-19 response. This ramp down includes elective surgical procedures and some outpatient clinics.
“This has allowed us to identify staff in those areas and to redeploy them to other areas in need,” says Damiano Loricchio, Director of Workforce Planning and Utilization. “We match these staff based on their skills with the areas of the hospital that need help. Everyone has been amazing through this process and understands we’re all hands on deck right now.”
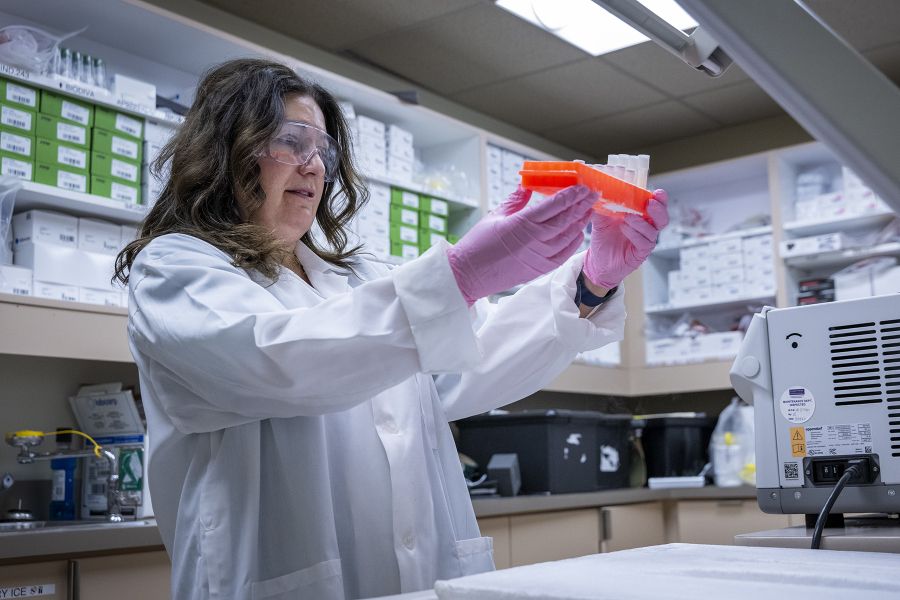
A major piece of this redeployment work is also ensuring that staff all have the right training to provide care in their new roles. This work is being led by KHSC’s professional practice team.
“We don’t want to force someone into a spot where they can’t succeed,” says Leanne Wakelin, Director of Professional Practice. “We provide them with onboarding and training, then schedule them for a few shifts with a ‘work-buddy’ from that area to ensure they’re feeling comfortable.”
Generally the approach is to provide someone with training to move to an area where patients have increasingly higher acute care needs. Staff from the outpatient ambulatory clinics have been trained and redeployed to work on medical/surgical units. Staff from medical/surgical units are trained to move to critical care areas.
So far, more than 40 people have been redeployed to Critical Care, and more than 60 within the Surgical Program. Another 30 have been assigned to a new High Intensity Nursing team that aims to help support the ICU, which typically runs on a one patient to one nurse ratio.
“This team acts as a buddy to the nurses in the ICU,” says Wakelin. “The high intensity nurse will do things like give medication and take blood. That then frees up the critical care nurse to do tasks that require different specialized training. They work together to care for the patient.”
Work is also underway to support allied health professionals on the front-line, with a current focus on Respiratory Therapists (RTs). That team is under added pressure as the number of patients requiring a ventilator due to COVID-19 is much higher than usual.
“We’ve been able to redeploy RTs from the Hotel Dieu Hospital (HDH) site as well as the Ontario Ventilator Equipment Pool located in Kingston,” says Wakelin. “We have also created a RT Assistant position that is being filled by RT students who have been hired on to support the team and complete tasks that are very specific based on their skillset.”
Nursing students have also been hired as nursing assistants on their off-days to help in other areas of the hospital, supporting nursing staff on inpatient units. They complete tasks like feeding and bathing patients and helping them make phone or video calls to families.
In the near future, KHSC will focus on setting up similar assistant positions for areas such as Physiotherapy (PT) and Occupational Therapy (OT).
“These critical-care patients won’t have an easy recovery ahead of them and will need a lot of support and rehabilitation before they are discharged. Allied health roles such as PT and OT will be critical areas of focus for us in the coming weeks,” says Wakelin.
Meanwhile, physicians from all areas of medical specialty are also working around the clock to ensure that care continues for our most urgent patients.
“Our physicians recognize this is a once in a lifetime crisis and they are stepping up to help any way they can,” says Dr. Fitzpatrick. “We’ve had many physicians step in to provide care in new spaces at HDH site and Providence Care. It’s been a real team effort from everyone in the organization.”
Wakelin agrees, “This has been a phenomenal organizational effort. There are problems that arise each day and people are finding ways around them for our patients. Our teams see the challenge they are up against and are putting themselves out there to say ‘with a little training I can do this and help out in areas where it’s really needed.”
Gallery


More than 200 people have been redeployed across KHSC