A synthetic stool treatment transplanted during a proof-of-concept trial at Kingston General Hospital has been shown to cure those who experience chronic C. difficile infections.
The results of the trial were published in Microbiome, a peer-reviewed scientific journal and were part of a co-authored study written by researchers at Kingston General Hospital’s Gastrointestinal Diseases Research Unit, Queen’s University, Guelph University and Western University.
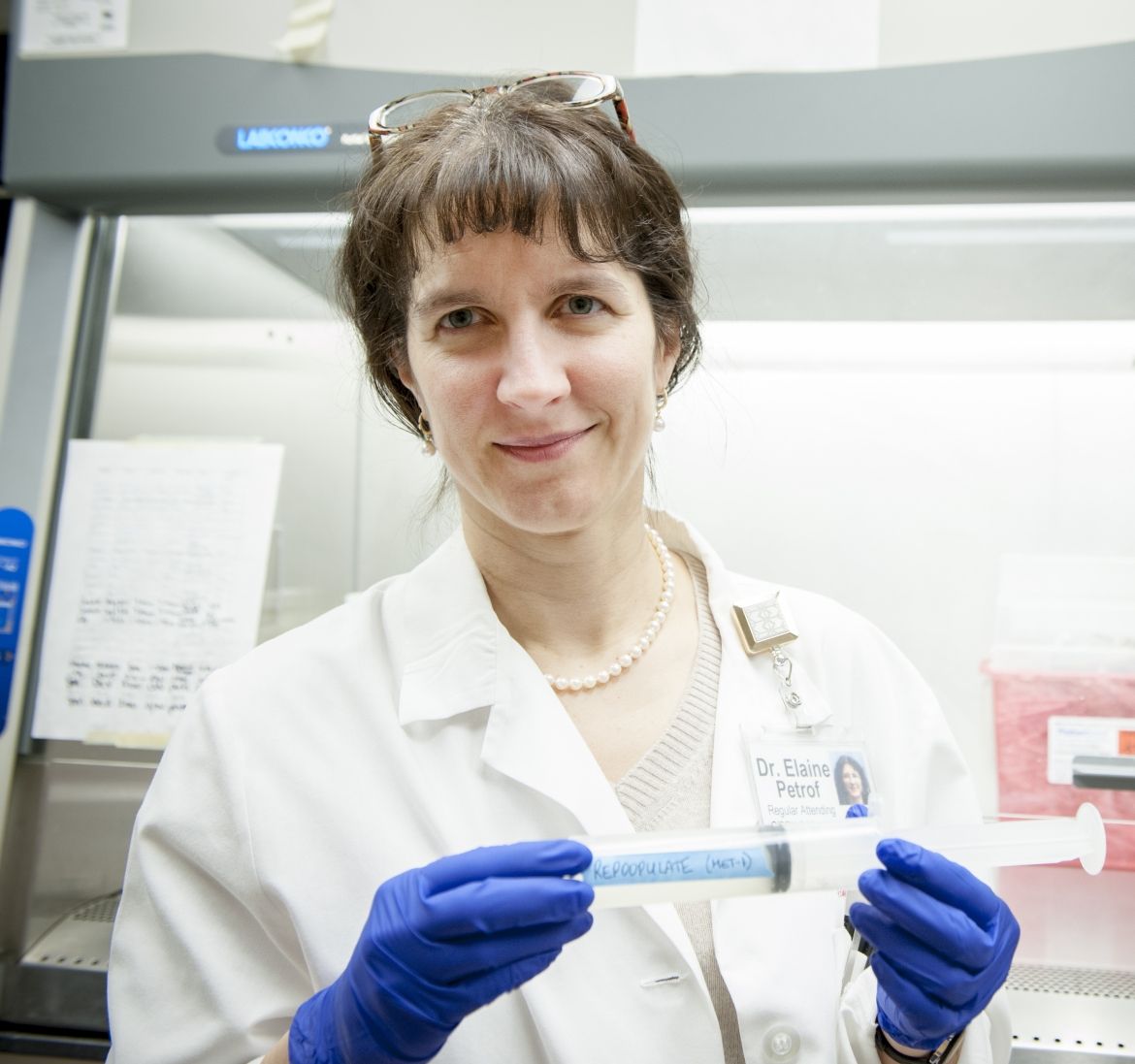
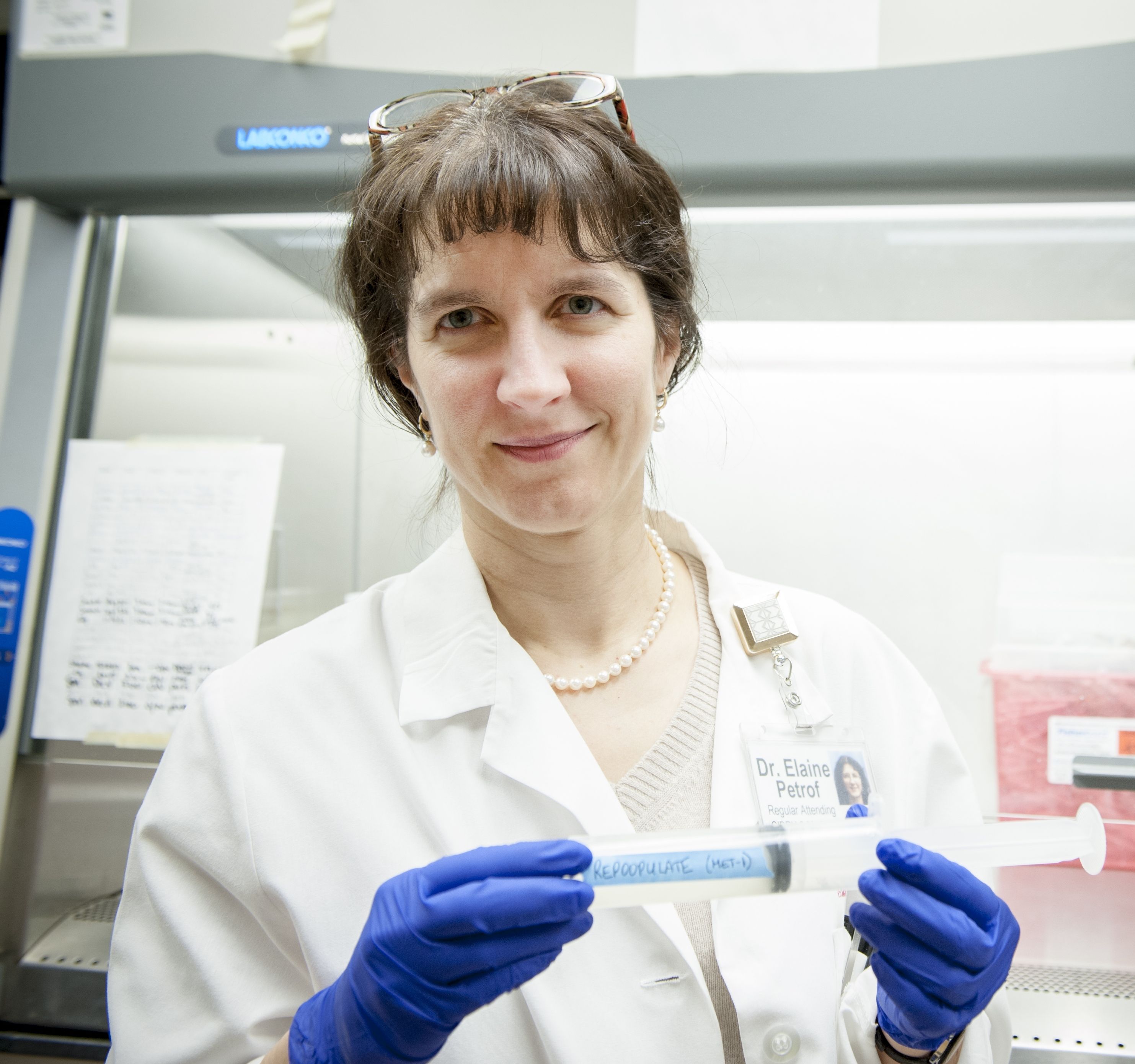
The researchers created synthetic stool, dubbed ‘Re-POOPulate’, to replace the need for human fecal matter used in stool transplants, a known treatment that has been successful in overcoming stubborn C. difficile infections. C. difficile is a toxin-producing bacterium that can result in severe gastrointestinal problems, and even death.
“Because the stool is synthetic, there is less of an ‘ick’ factor associated with the transplant,” says Dr. Elaine Petrof, an Infectious Diseases Specialist with the Gastrointestinal Diseases Research Unit at Kingston General Hospital. “Re-POOPulate has the potential to become a more attractive treatment for those experiencing this debilitating infection.”
The synthetic stool is made from purified intestinal bacterial cultures grown using the “Robo-gut” machine housed in Guelph microbiologist and study co-author Emma Allen-Vercoe’s lab. The treatment works as a ‘super probiotic’ for the gut.
The synthetic stool treatment was tested in two patients with recurring C. difficileinfections at Kingston General Hospital. “Both patients experienced relief of their symptoms within three days of treatment and tested negative for C. difficile six months later. They responded very well and seem to be completely cured,” says Petrof.
The potential this treatment has to help C. difficile sufferers is “exciting”, says Petrof. “Our hope is that this could become an alternate therapy for treating C. difficile. It has many benefits, including being safer for patients and medical staff as well as being easily and quickly reproduced based on a patient’s needs,” says Petrof.
Petrof collaborated on the study with Allen-Vercoe, Dr. Stephen Vanner, head of the Gastrointestinal Disease Research Unit at Kingston General Hospital and Queen’s University, Gregory Gloor, a biochemistry professor at the University of Western Ontario and Guelph pathobiology professor Scott Weese.