In a bustling conference hall in 2019, Dr. Omar Islam came across a groundbreaking innovation that would, in just a few years' time, revolutionize medical imaging in remote communities.
"They were in a tiny corner of this massive conference hall, doing a demo with cantaloupes and watermelons. It was brand new," he recalls.
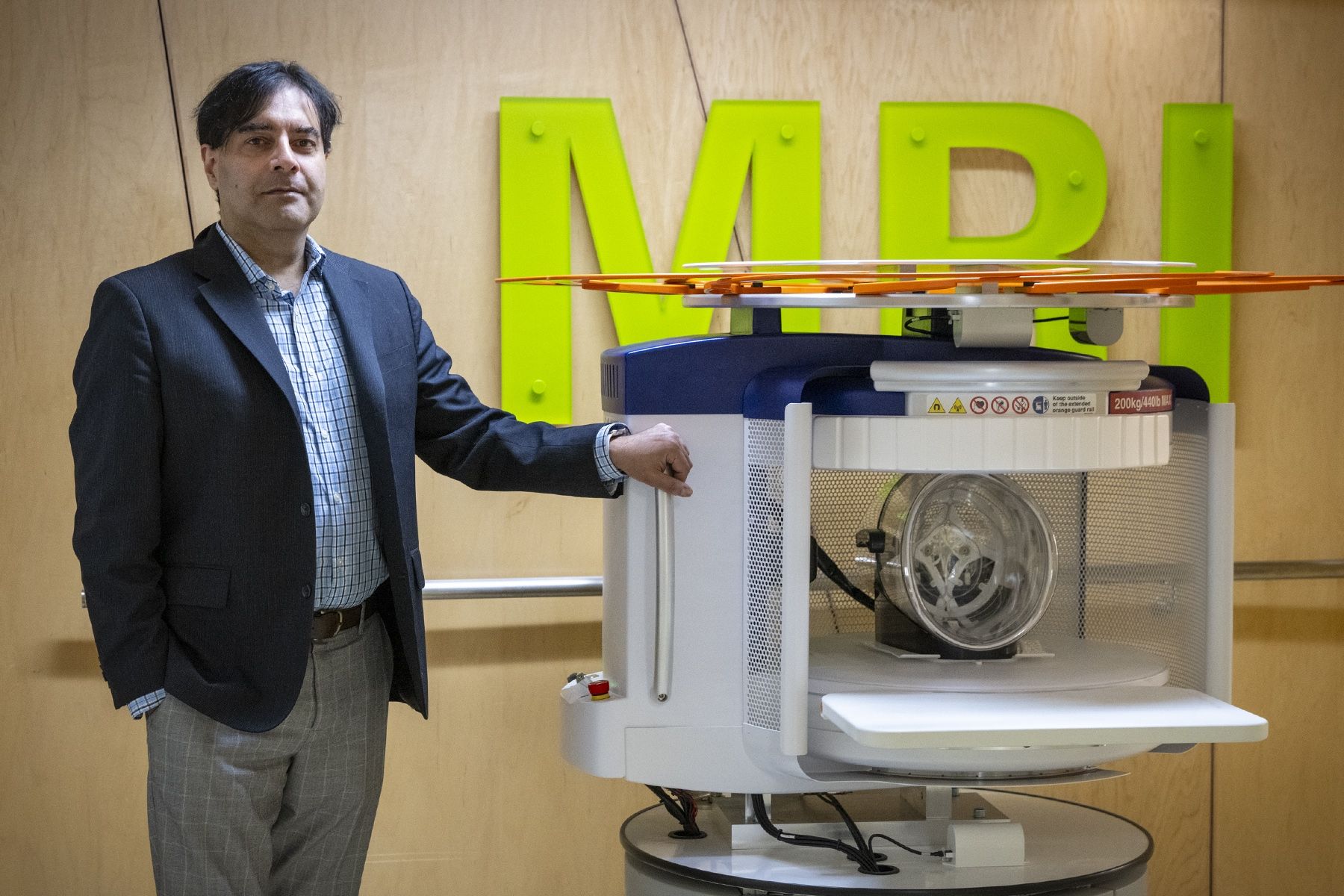
That machine was a portable MRI, and since that chance encounter in 2019, Kingston Health Sciences Centre (KHSC) and Dr. Islam have become leaders in adopting this revolutionary new technology.
Dr. Islam’s major focus is on fair access to medical care, specifically medical imaging, and he could see the potential of the portable MRI right away.
It's this small machine on wheels that uses about the same amount of energy as a coffee machine, and you could see it rolling through mountains in Pakistan, or small villages in Africa.
It’s estimated that between 30 and 40 per cent of the world’s population doesn’t have access to MRI scanning, and when there is access, it’s extremely expensive. This is primarily the case for low-middle-income countries, but there are communities everywhere, including remote areas in Canada, where geography is still a big barrier.
The Swoop MRI was originally designed for ICUs to reduce the impacts of transporting patients to imaging suites – it's why KHSC recently got its first device – but Dr. Islam thought it could also be used to close the healthcare gap, being used to do advanced brain imaging in remote, primarily Indigenous communities.
Weeneebayko General Hospital, located in Moose Factory, Ontario, is a 2.5-hour flight from Kingston. The hospital has an agreement with Queen’s University and KHSC who provide tertiary level care. This means that patients are routinely sent to Kingston for certain procedures, including MRI scans.
The process is time-consuming, resource-intensive and expensive. It costs approximately $17,800 to transfer a patient from the north to KHSC. A nurse needs to accompany the patient, causing downstream staffing issues and, most importantly, the process is extremely disruptive for the patients and their families.
It became clear that a portable MRI in Moose Factory was the perfect solution.
"We put a proposal together with former Dean Dr. Jane Philpott, connected with the chief of staff and CEO at Moose Factory, and presented this to the manufacturer, Hyperfine," says Dr. Islam, who is the head of the Department of Radiology at KHSC and Queen’s University. "They thought it was a great idea and never thought of this in a remote setting. Literally the next day, Hyperfine said, 'Here’s the size of our crate, how do we ship it?'"
But there were many steps that needed to be completed before it could be shipped. Dr. Islam and the team worked to obtain approval from Health Canada. They also made sure KHSC’s IT infrastructure could handle receiving and processing scans from the machine in the north. Perhaps the most important step was educating the local community in Moose Factory on portable MRI and obtaining their approval.
One of the big issues was ‘why us?’ The community didn’t want to be used to test experimental technology, so we provided answers to their questions and went on a local radio show broadcast in English and Cree to talk about its safety and show the potential benefits.
With everyone now onboard, the machine was shipped to Moose Factory, with full approval from Health Canada to scan 50 patients in its first year.
"We knew the machine would provide reliable results, but we also needed to know doing scans remotely would make a difference economically, so we performed an economic feasibility study – the only one of its kind for portable MRI."
The results were dramatic. The machine was able to produce high quality images for medical teams and could save $7.8 million over five years compared to flying patients to KHSC.
The study was published a year ago and showed that it’s a ‘no brainer’ for scanning patients in remote communities.
The findings were so profound that a private donor in Moose Factory stepped forward to buy one once the trial period ended – ensuring access for the community for the foreseeable future.
Moose Factory was the first community in Canada to receive a portable MRI. Now there are seven units in place across the country. The approach is catching on – Nunavut recently received a portable MRI with hopes to implement a similar care model.
"My dream would be to have these in every remote community in Canada. There are hundreds of places like Moose Factory across our vast country, and portable MRI would really democratize access to care."



